Diabetes is a growing problem in the United States. An estimated 29 million Americans (9.3% of the population) currently have diabetes, and by 2050, the Centers for Disease Control and Prevention predict that number will rise to as many as one in three adults. As a health and fitness professional, you likely work with clients who have type 2 diabetes. To kick off Diabetes Awareness Month, here are six important factors to consider when working with clients with type 2 diabetes.
1. Obtain Medical Clearance
According to the American College of Sports Medicine’s Risk Stratification Criteria, clients with a known metabolic disease should receive a medical exam prior to engaging in physical activity. This step is often overlooked among those with type 2 diabetes because it has become so common. While exercise will benefit individuals with type 2 diabetes, certain medical precautions may be required. Obtaining medical clearance before exercise ensures that both you and your client stay safe.
2. Monitor Blood Sugar
At the onset of exercise, the body breaks down stored glycogen for energy, and muscle cells become more receptive to glucose. In individuals with diabetes, the ability to uptake glucose is compromised, which can lead to more extreme blood-sugar responses to exercise. With very high-intensity exercise, the liver may break down glycogen more rapidly than the muscle cells can uptake it, causing an initial increase in blood glucose levels. In other cases, blood glucose levels may fall too rapidly, putting individuals at risk for low blood sugar or hypoglycemia.
Monitoring blood sugar before, during and after exercise can help ensure clients avoid dangerous complications. Exercise should be postponed or discontinued if blood glucose levels fall below 100 mg/dL or rise above above 300 mg/dL or 250 mg/dL with the presence of ketones. It’s important to remind clients to pay careful attention to blood sugar levels in the few hours after exercise as well, as post-exercise hypoglycemia can also occur due to the body’s increased susceptibility to insulin.
Be prepared for bouts of hypoglycemia with fast-acting carbohydrate sources such as juice or raisins. Additionally, encourage clients to stay adequately hydrated, as blood glucose is negatively impacted by dehydration.
3. Track Changes
As described earlier, type 2 diabetes is characterized by an impaired sensitivity to insulin, making the cells of the body less able to utilize glucose. For this reason, exercise is an excellent way to combat type 2 diabetes because it increases insulin sensitivity, both immediately and long-term. This can be a huge motivator for clients who believe that their diabetes is unmanageable without the use of medication. To illustrate the effects of exercise on blood sugar, ask your clients to keep a blood sugar log with pre- and post-exercise blood-sugar measurements.
Clients can also track their mood and energy in relation to exercise sessions. The association between regular physical activity and increased energy can be a huge motivating factor. Over time, this can help clients see the positive effect exercise has on their blood sugar levels and encourage them to continue their exercise regimens.
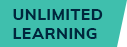
4. Include Resistance Training
Much of the talk around exercise and diabetes centers on cardiorespiratory exercise. However, resistance training also has powerful blood sugar-lowering effects. Resistance training increases muscles’ sensitivity to insulin, allowing them to take in more glucose. Increased skeletal muscle mass that can occur with resistance training will yield further improvements in glucose uptake. The American College of Sports Medicine and American Diabetes Association recommend that individuals with type 2 diabetes perform resistance training at least two, but preferably three, days per week, focusing on all major muscle groups.
5. Promote After-meal Movement
Research suggests that small amounts of exercise immediately following meals can be more effective for blood-sugar management with diabetes than one single daily bout of exercise. One study compared the blood-sugar effects of a 30-minute daily walk to three 10-minute bouts immediate following meals. The researchers found that the three 10-minute bouts resulted in significantly lower daily blood-sugar levels than one 30-minute session. This effect was particularly pronounced after dinner, when the greatest amounts of carbohydrates were eaten and individuals were most sedentary.
6. Don’t Call Them Diabetics
Though the terms “type 2 diabetic” and “individual with type 2 diabetes” may seem to be interchangeable, each confers different meaning. Referring to a client as a type 2 diabetic assigns diabetes as part of his or her identity. When looking to adopt behaviors to manage or reverse diabetes, labeling individuals as diabetics may make them feel less capable of change. Conversely, referring to someone as an individual “with type 2 diabetes” implies a transient state, similar to that of a “person with the flu.” This subtle shift in terminology can empower your clients to take action to manage or reverse their diabetes through lifestyle modifications.
By understanding the exercise guidelines associated with type 2 diabetes, you can better help your clients adopt exercise habits that allow them to improve their health and manage or reverse their diabetes.




 by
by