
By Lance Dalleck, Ph.D.
High-intensity interval training (HIIT) involves alternating brief bouts (30 seconds to 5 minutes) of higher-intensity sessions with either rest or lower-intensity workloads throughout an exercise routine. HIIT has traditionally been used to train athletes requiring high levels of both aerobic and anaerobic fitness. Recently, numerous randomized, controlled studies have demonstrated the safety and effectiveness of HIIT in clinical populations (Munk et al., 2009; Nilsson, Westheim and Risberg, 2008). Interestingly, results from these trials also demonstrate that HIIT can induce significantly greater improvements in cardiorespiratory fitness and other physiological parameters when compared to moderate-intensity, continuous training, which is traditionally prescribed for clinical populations (Cornish, Broadbent and Cheema, 2011). Such findings are important for many reasons, and this article provides fitness professionals with a detailed guide for designing and implementing HIIT programs for clients with common clinical conditions.
The Scientific Evidence for HIIT
The widespread physical-activity recommendation for American adults is 150 minutes per week of moderate-intensity exercise. Completion of this weekly amount of exercise confers numerous health benefits. Unfortunately, the majority of American adults fall short of recommended physical-activity guidelines, with lack of time cited as the primary barrier to achieving weekly exercise goals. It is largely for this reason that the scientific community first considered HIIT as a viable option for clinical populations. Could HIIT be a time-efficient strategy for improving health? A growing body of evidence suggests that this innovative approach to exercise programming yields training adaptations comparable, and superior, to traditional, moderate-intensity exercise. Here are five key studies:
- Norwegian researchers (Rognmo et al., 2004) compared the effectiveness of 10 weeks of HIIT to moderate-intensity continuous training in cardiac-diseased individuals. The HIIT program consisted of four interval bouts of four minutes at 80 to 90% maximal oxygen uptake (VO2max), interspersed with four minutes of active recovery at 50 to 60% VO2max, for three sessions per week. It was reported that VO2max increased by 10% more in the HIIT group.
- Canadian researchers (Warburton et al., 2005) compared the effectiveness of 16 weeks of HIIT to traditional moderate-intensity continuous training in cardiac-diseased individuals. The HIIT program entailed nine interval bouts of two minutes at 90% heart-rate reserve (HRR)/oxygen uptake reserve (VO2R), interspersed with two-minute active recovery bouts at 40% HRR/VO2R, for two sessions per week. It was found that VO2max increased by 5% more in the HIIT group.
- Another group of Norwegian researchers (Wisloff et al., 2007) compared the effectiveness of 12 weeks of HIIT to traditional, moderate-intensity continuous training in cardiac-diseased individuals. The HIIT program consisted of four interval bouts of four minutes at 90 to 95% maximal heart rate (HRmax), interspersed with three-minute active recovery bouts at 50 to 60% HRmax, for three sessions per week. It was found that VO2max increased by 30% more in the HIIT group.
- A third group of Norwegian researchers (Tjonna et al., 2008) investigated the effectiveness of 16 weeks of HIIT compared to traditional, moderate-intensity continuous training as a treatment for individuals with metabolic syndrome. The HIIT program consisted of four interval bouts of four minutes at 90% HRmax, interspersed with three-minute active recovery bouts at 70% HRmax, for three sessions per week. Researchers concluded that HIIT was superior to moderate-intensity continuous training at improving endothelial function, blood glucose control and fat metabolism.
- More recently, a group of Canadian researchers (Little et al., 2011) investigated the effects of two weeks of low-volume HIIT on metabolic health in a group of individuals with type 2 diabeties. The HIIT program consisted of 10 interval bouts of 60 seconds at 90% HRmax, interspersed with 60 seconds of passive rest or very-light active recovery, for three sessions per week. After just six total exercise sessions, subjects’ blood glucose control was significantly improved.
Collectively, these findings suggest that HIIT may serve as an effective substitute for, or adjunct to, commonly recommended moderate-intensity exercise training.
Making HIIT Safe for Clinical Populations
Safety is the first issue that must be addressed prior to designing and implementing a HIIT program. In general, exercise is safe for most individuals, and exercise, by itself, does not incite adverse cardiovascular or other untoward events. The risk of an acute myocardial infarction or sudden death during exercise is higher in adults compared to their younger counterparts; the greatest risk exists for those individuals with underlying or diagnosed cardiovascular disease. The absolute risk of sudden death during vigorous-intensity physical activity has been estimated to be one per year for every 15,000 to 18,000 people (ACSM, 2010). In terms of HIIT, a recent review of studies, which included a HIIT intervention for patients with cardiovascular disease, reported no adverse cardiac or other life-threatening events secondary to participation in HIIT (Cornish, Broadbent and Cheema, 2011).
The key to minimizing complications during and after exercise is to identify those individuals who may be at an increased risk of adverse symptoms through appropriate pre-participation screening. It must be assumed that any individual with a clinically relevant cardiovascular disease risk factor or diagnosed cardiovascular disease requires both a medical examination and a physician-supervised maximal exercise test prior to participation in HIIT (ACSM, 2010). These procedures will pinpoint contraindications to HIIT. For instance, an individual who terminates a maximal exercise test prematurely due to chest discomfort or dizziness would not be a candidate for HIIT. Ideally, you should also provide your clients with a detailed description of the HIIT program that can be reviewed and approved by their physicians. In summary, an appreciation for the risk involved with HIIT, as well as a clear understanding of the importance of comprehensive screening prior to client participation in HIIT, are vital measures in risk management.
Monitoring
Pre-screening, however, is only one part of ensuring a safe and effective HIIT program. Appropriate monitoring procedures also are obligatory. Consider the following three essential categories of monitoring:
- Proper preparation and recovery: The physiological and psychological demands of HIIT are greater compared to moderate-intensity continuous training. This means clients need to be sufficiently prepared for these sessions in advance and understand the importance of recovery upon completion of the training session. Areas that take on increasing importance include proper hydration and nutrition, appropriate exercise attire and a complete warm-up routine. Likewise, following the interval session, clients should perform a complete cool-down and then rehydrate and refuel in a timely manner. Closely monitor your clients to ensure that each of these preparatory and recovery steps is being accomplished.
- Adherence to target exercise intensity: Confirming that your clients are performing the correct exercise intensity is always a primary concern; however, when performing HIIT this consideration is amplified. Whether the method for recommending exercise intensity is established by rating of perceived exertion (RPE), workload (e.g., treadmill speed) or target heart rate (e.g., % of HRR), it is paramount that you carefully monitor the HIIT sessions and verify that actual exercise intensity is aligned with target intensity. Simply put, there is less margin for error with HIIT. Although a subtle increase in exercise intensity, initiated by the client, during a specific interval bout may at first glance seem inconsequential, in actuality it may be the difference between a high-intensity workload and an all-out workload.
- Knowledge of criteria for terminating exercise: Provided clients have been sufficiently screened, prepared properly in advance of HIIT and adhere to the target exercise intensity, the likelihood of an adverse event is greatly diminished. Nevertheless, there is one additional measure required to optimize safety. It is essential that you are able to recognize, and also educate your clients to recognize, general indications for terminating exercise. Chest discomfort, failure of heart rate to increase normally with increased workload, lightheadedness, severe fatigue and shortness of breath are all abnormal responses to exercise, and warrant the termination of exercise that day.
Essential Nuts and Bolts of a HIIT Program
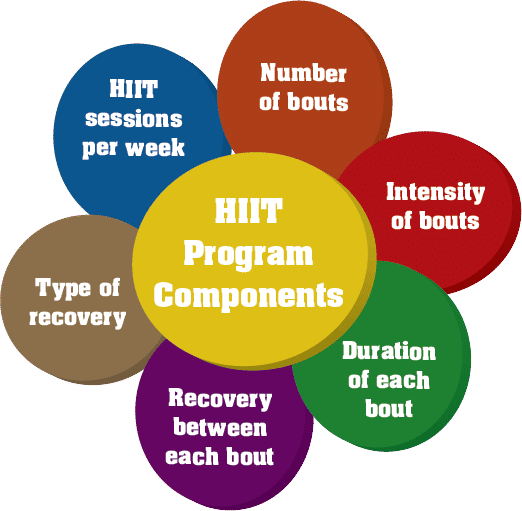
Consider the following six components when designing HIIT programs for clients (Figure 1):
- HIIT sessions per week: Two to three HIIT sessions per week are commonly employed in research and, therefore, should be the goal in a real-world setting.
- Number of bouts: This component refers to how many interval bouts will be performed during each HIIT session (e.g., six bouts of 60 seconds each).
- Intensity of bouts: The intensity of each interval bout of the HIIT session can be quantified using various methods, including a percentage of maximal heart rate (e.g., 85 to 90% HRmax).
- Duration of each bout: This component refers to the length (time or distance) of each interval bout. For instance, each interval bout could be four minutes or 800 meters.
- Recovery between each bout: This component refers to the length (time or distance) between each interval bout. For instance, recovery between each interval bout equates to four minutes.
- Type of recovery between each bout: The type of recovery performed between each interval bout is generally either active or passive. Active recovery comprises continued exercise, but at a substantially lower intensity. Passive recovery consists of resting completely between interval bouts in either a standing or sitting position.
Figure 1. HIIT Program Components
Programming, Progression and Maintenance
Initially, previously untrained clients should perform a proper base-building phase, consisting of regular moderate-intensity exercise. The increase in training volume during this phase should be approximately 10 percent to 20 percent per week (ACSM, 2010). For example, if an individual is currently walking 5 miles per week, the increase in training volume should be no more than 1 mile per week. Incorporating multiple training modalities into the aerobic exercise routine may also facilitate program adherence. The maximum training volume an individual attains can be best gauged by determining the overall capacity and motivation of your client. Research suggests that, in a dose-response manner, the higher the training volume, the greater the improvement in various health outcomes (ACSM, 2010). The base-building phase should be a minimum of three months for clinical populations. Provided a client has physician approval, as discussed previously, it is now appropriate to gradually introduce HIIT sessions into the program. HIIT recommendations are presented in Table 1.
| Table 1. HIIT Recommendations for Clinical Populations |
| Program Component |
Program Modification |
| Frequency |
Two HIIT sessions per week |
| Exercise Intensity |
85–95% of maximal heart rate (HRmax) |
| Bouts/Session |
Inversely related to duration of HIIT bouts:
• 4 bouts/session if duration of HIIT bout is 4 minutes
• 8 bouts/session if duration of HIIT bout is 2 minutes
• 10 bouts/session if duration of HIIT bout is 60 seconds
|
| Duration of Bouts |
4 minutes, 2 minutes or 60 seconds |
| Recovery Length |
Greater than, or equivalent to, the duration of each HIIT bout. For example, if the duration of the HIIT bout is 60 seconds, the recommended recovery length is 2 minutes; if the duration of the HIIT bout is 4 minutes, the recommended recovery length is 4 minutes. |
| Type of Recovery |
Active recovery at low intensity (e.g., 50–70% HRmax) is strongly recommended over passive recovery. |
Interval workouts are high-intensity training sessions performed for short durations at velocities or workloads near maximal. Accordingly, these sessions must include both a proper warm-up (with a minimum of five to 10 minutes of light aerobic exercise) and cool-down. The first step in determining the intensity component of HIIT is to obtain a valid measurement of your client’s maximal heart-rate values. Accurate monitoring of HIIT intensity is also essential. A heart-rate monitor, or the ability to accurately palpate heart rate, can ensure that actual exercise intensity corresponds to the recommended exercise intensity during HIIT sessions.
The earlier evidence presented suggests that the proper duration of these interval work bouts ranges from two to four minutes, with similar amounts of time for recovery between bouts. Initially, the number of interval repetitions may only be one or two per session and progress by one additional repetition per week. Ultimately, the total number of repetitions should consist of four to 10 repetitions, depending on the duration and training intensity of the interval bouts. Research has shown that a gradual increase in interval repetitions over a one-month timeframe is a successful progression strategy (Dalleck et al., 2010).
The total number of HIIT sessions per week can also progress over time. Initially, a single HIIT session per week is the proper starting point. Once your client has successfully progressed to the target interval bouts per session and maintained that level for approximately one month, it may be appropriate to add an additional HIIT session to the weekly program. Importantly, the progression of interval bouts for the second HIIT session should follow the same format as the preliminary one. In the long run, research suggests three HIIT sessions per week may be feasible (Cornish, Broadbent and Cheema, 2011). However, given the relative novelty of HIIT for clinical populations, a more conservative approach of one to two sessions per week, performed on non-consecutive days, is recommended. It is also important to note that, while HIIT sessions will replace one or two moderate-intensity training sessions, they should be perceived as a complement to moderate-intensity training. Clients should still aim for three to five days per week of moderate-intensity aerobic training.
After progression has been made to target HIIT parameters (e.g., number of interval bouts per session), these training parameters will be maintained long-term. The temptation to increase interval bouts per session, interval intensity and/or HIIT sessions per week should be avoided, as it will likely lead to overtraining and/or injury. Alternatively, you may elect to modify HIIT parameters (e.g., from four bouts of four minutes to eight bouts of two minutes) to maintain your client’s interest and motivation; however, the top-end recommendations listed in Table 1 for each parameter should still be observed.
References
American College of Sports Medicine (2010). ACSM’s Guidelines for Exercise Testing and Prescription (8th ed.). Baltimore, Md.: Wolters Kluwer/Lippincott Williams & Wilkins.
Cornish, A.K., Broadbent, S. and Cheema, B.S. (2011). Interval training for patients with coronary artery disease: A systematic review. European Journal of Applied Physiology, 111, 579–589.
Dalleck, L. et al. (2010). Dose-response relationship between interval training frequency and magnitude improvement in lactate threshold. International Journal of Sports Medicine, 31, 567–571.
Little, J.P. et al. (2011). Low-volume high-intensity interval training reduces hyperglycemia and increases muscle mitochondrial capacity in patients with type 2 diabetes. Journal of Applied Physiology, 111, 1554–1560.
Munk, P. et al. (2009). High-intensity interval training may reduce in-stent restenosis following percutaneous coronary intervention with stent implantation: A randomized controlled trial evaluating the relationship to endothelial function and inflammation. American Heart Journal, 158, 734–741.
Nilsson, B., Westheim, A. and Risberg, M. (2008). Effects of group-based high-intensity aerobic interval training in patients with chronic heart failure. American Journal of Cardiology, 102, 1361–1365.
Rognmo, O. et al. (2004). High-intensity aerobic interval exercise is superior to moderate-intensity exercise for increasing aerobic capacity in patients with coronary artery disease. European Journal of Cardiovascular Prevention and Rehabilitation, 11, 216–222.
Tjonna, A.E. et al. (2008). Aerobic interval training versus continuous moderate exercise as a treatment for the metabolic syndrome: A pilot study. Circulation, 118, 346–354.
Warburton, D.E.R. et al. (2005). Effectiveness of high-intensity interval training for the rehabilitation of patients with coronary artery disease. American Journal of Cardiology, 95, 1080–1084.
Wisloff, U. et al. (2007). Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: A randomized study. Circulation, 115, 3086–3094.
____________________________________________________________________
 Lance C. Dalleck, Ph.D., is academic coordinator of the Cardiac Rehabilitation postgraduate program at the University of Auckland in New Zealand. His research interests include improving exercise performance and health outcomes through evidence-based practice, quantifying the energy expenditure of outdoor and non-traditional types of physical activity, and studying historical perspectives in health, fitness and exercise physiology.
Lance C. Dalleck, Ph.D., is academic coordinator of the Cardiac Rehabilitation postgraduate program at the University of Auckland in New Zealand. His research interests include improving exercise performance and health outcomes through evidence-based practice, quantifying the energy expenditure of outdoor and non-traditional types of physical activity, and studying historical perspectives in health, fitness and exercise physiology.