An estimated 14.2 million Americans—about one in 20—live with chronic obstructive pulmonary disease (COPD), according to data from the Centers for Disease Control and Prevention. COPD is a condition stemming from damage to the airways and other parts of the lung. This damage results in inflammation and other problems that impede airflow and make it challenging to breathe. COPD symptoms include chest tightness, shortness of breath, varying degrees of difficulty breathing, and coughing that produces large amounts of mucus.
The sixth leading cause of mortality in the United States, COPD is comprised of chronic bronchitis and/or emphysema. A higher prevalence of COPD has been shown in the following groups: rural residents, older adults (age 65 years and older) and persons with a previous history of smoking. Indeed, the single greatest risk factor for COPD is tobacco smoking. COPD is frequently accompanied by weight loss, sarcopenia, and an eventual decrease in muscular strength and endurance. Reduced overall fitness can lead to a downward spiral that ultimately culminates in disability and diminished activities of daily living (ADLs).
Fortunately, as a health and exercise professional, you can work closely with clients who have COPD to design and implement exercise programs that minimize symptoms, maintain ADLs and improve quality of life. This article outlines strategies for helping clients who have COPD exercise safely and effectively.
Common Medication–exercise Response Interactions and Exercise Program Modifications
The medical management of COPD can include a broad range of medications, and it is critical that you understand how certain medications interact with an individual’s response to exercise and how the exercise program might need to be adjusted. For example, short- and long-acting beta agonists (i.e., bronchodilators) are commonly prescribed for COPD. These medications help relax and open the airways. However, bronchodilators can also elicit increases in heart rate and blood pressure. As such, additional monitoring of blood pressure may be warranted. Additionally, the use of target heart rate based on age-predicted maximal heart rate is not advised given the potential side effects of COPD control medications.
Clients with COPD are also likely to be taking corticosteroids, which are powerful anti-inflammatory medications used to lessen the severity of exacerbations and provide long-term COPD control. A side effect of corticosteroids is muscle atrophy, so it is important to encourage clients to perform muscular training to help counteract these unwanted muscle-wasting side effects.
The intent of this section is not to be exhaustive in its scope. Rather, it’s to highlight the concept of medication–exercise responses and reinforce the importance of making appropriate program-design adjustments that better serve your clients who have COPD. It’s also critical to collaborate with other medical providers that help your clients manage their COPD and familiarize yourself with other relevant medications and considerations for overall exercise programming.
Exercise Programming for Clients Who Have COPD
Overall, exercise is well tolerated in people with COPD and should be encouraged. In particular, muscular training can help lessen the deleterious effects of the muscle atrophy that frequently accompanies COPD. In most cases, you can follow the exercise guidelines presented in Table 1 for cardiorespiratory and muscular training with your clients who have COPD.
Table 1. Exercise Guidelines for Clients With COPD
|
Cardiorespiratory Training
|
|
Frequency
|
3–5 days per week
|
|
Intensity
|
Initially below VT1 and progress to intensities from VT1 to just below VT2
Moderate-to-vigorous
RPE 4–6 (0–10 scale)
50–80% peak work rate
|
|
Time
|
20–60 minutes per day at moderate-to-high intensities, as tolerated
≥20 minutes of exercise with intermittent recovery periods of lower intensity work or rest
|
|
Type
|
Walking
Cycling
Upper-body ergometry
|
|
Progression
|
Progress following the ACE Integrated Fitness Training® Model based on client goals and availability.
|
|
Muscular Training
|
|
Frequency
|
A minimum of 2 nonconsecutive days per week
|
|
Intensity
|
60–70% 1-RM for beginners to build muscular strength
≥80% 1-RM for experienced weightlifters
<50% 1-RM for muscular endurance
|
|
Time
|
2-4 sets of 8–12 repetitions for muscular strength
≤2 sets of 15–20 repetitions for muscular endurance
|
|
Type
|
All major muscle groups
Free weights
Body-weight exercises
Weight machine
|
|
Progression
|
Progress following the ACE Integrated Fitness Training Model based on client goals and availability.
|
Note: VT1 = First ventilatory threshold; VT2 = Second ventilatory threshold; RPE = Rating of perceived exertion; 1-RM = One-repetition maximum
Source: American College of Sports Medicine (2022). ACSM’s Guidelines for Exercise Testing and Prescription (11th ed.). Philadelphia: Wolters Kluwer.
There are, however, a number of special programming considerations to keep in mind:
- Closely monitor initial exercise sessions to ensure your client is correctly performing all exercises.
- Ensure that your client’s preliminary exercise sessions are designed to align duration and intensity with their tolerance and symptoms.
- Monitor oxygen saturation levels with pulse oximetry during initial exercise sessions to avoid desaturation of blood oxygen levels. Additionally, it is helpful to identify the specific workloads at which desaturation occurs and establish this threshold as a ceiling in terms of exercise intensity. Finally, establish and maintain communication with your client’s medical team with respect to a specific oxygen saturation exercise termination threshold (e.g., ≤88%).
- Clients should be encouraged to initially exercise below the first ventilatory threshold (VT1). Use the talk test to identify your client’s personal VT1 values. Higher exercise intensities have been shown to confer greater physiological adaptations, so gradually progress intensity from a client’s VT1 to second ventilatory threshold (VT2) values, if they are able to tolerate the increased exercise intensity.
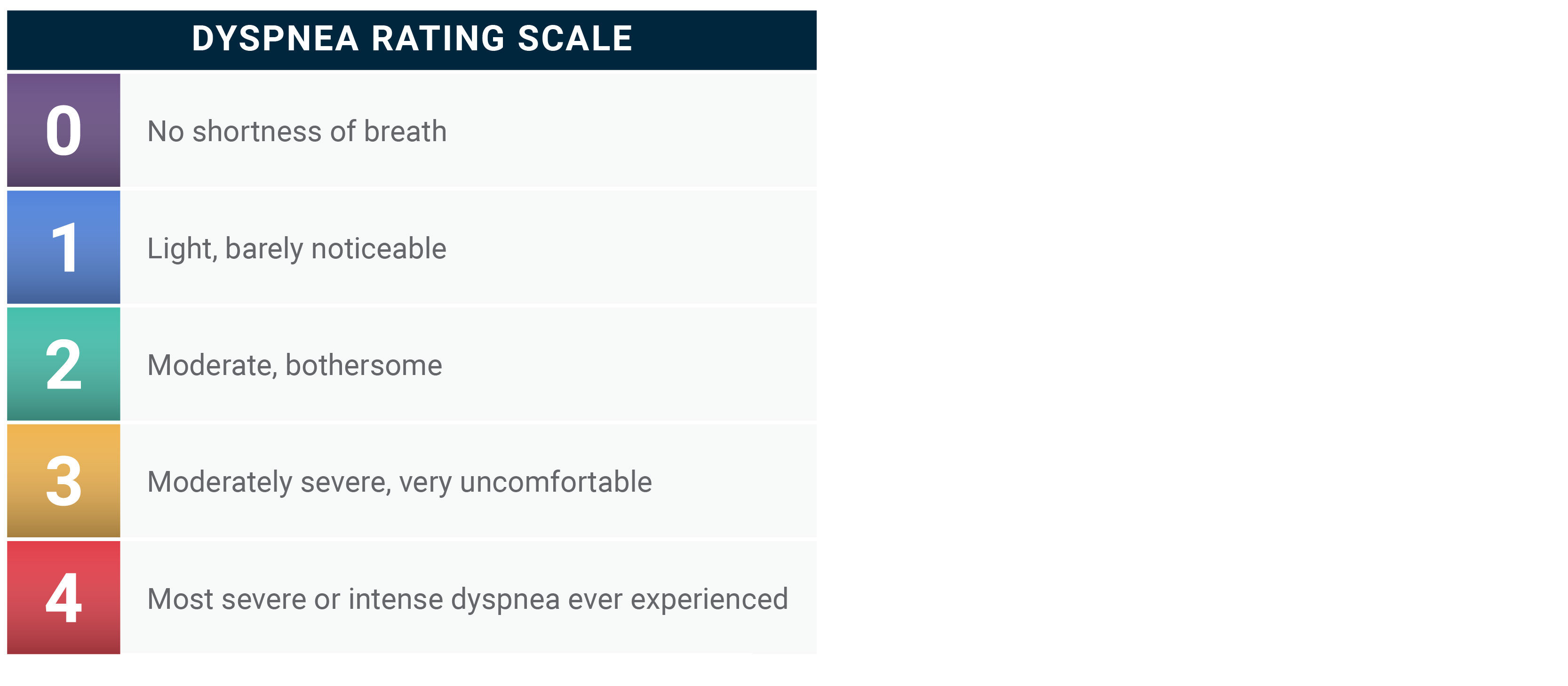
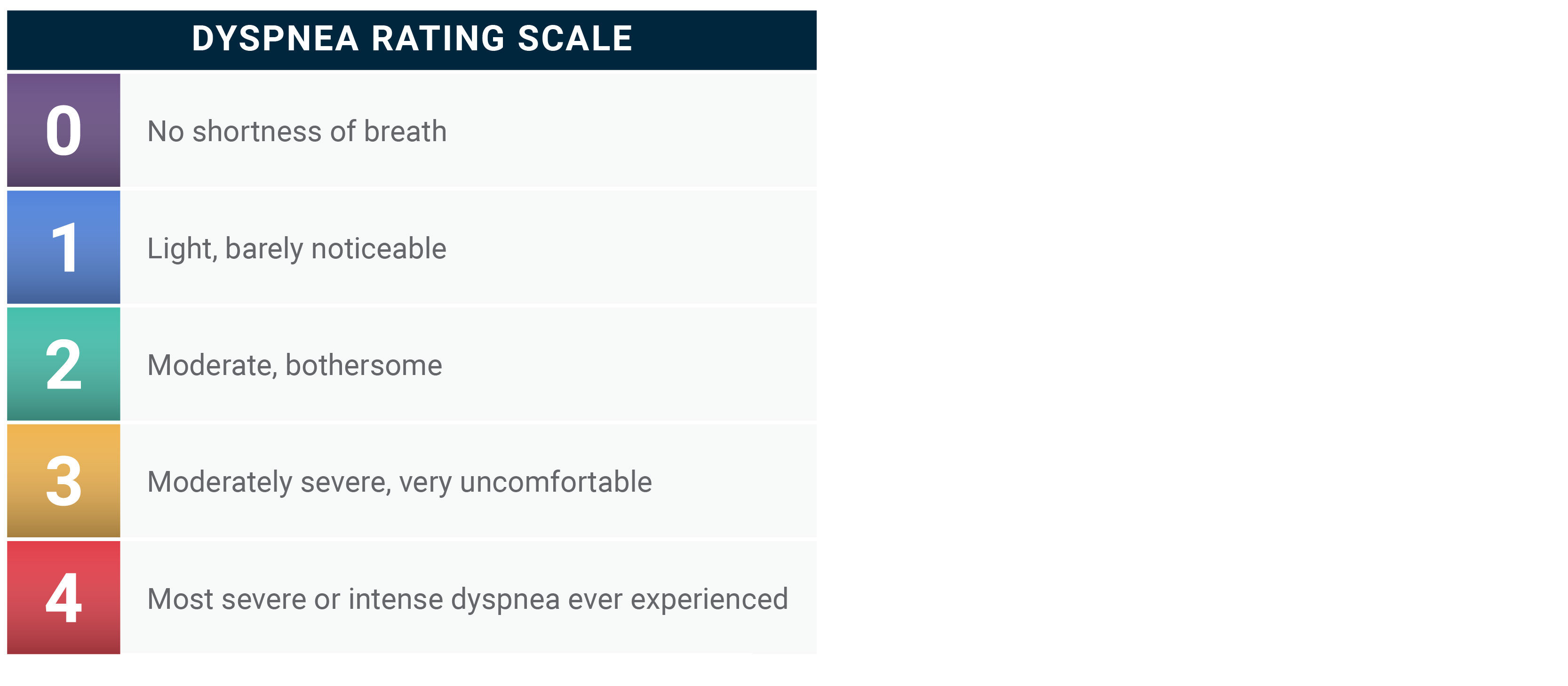
- Closely monitor the severity of symptoms throughout the exercise sessions. In this regard, the dyspnea scale shown in Table 2 can be a helpful guide for clients to monitor their symptoms and keep the duration and intensity of exercise appropriate. As a general rule, a dyspnea rating of 1 to 2 on the 0-to-4 scale will coincide with a client’s VT1 and VT2 values.
- The pathophysiology of COPD can lead to postural deficiencies that limit mobility in the thoracic region. As such, corrective and flexibility exercises are beneficial. The general frequency, intensity, time and type (FITT) approach to exercise programming used for cardiorespiratory and muscular-training program design can also be applied to flexibility exercise programming. Flexibility training should be performed on at least two to three days per week with daily being most effective. Each stretch should be performed for two to four repetitions and static stretched should be held at a point of slight discomfort 10 to 30 seconds. Be sure to encourage gentle, progressive stretching to avoid over-stretching. Tai chi and yoga may also be effective modalities of physical activity that incorporate flexibility and breathing exercises.
- As mentioned earlier, clients with COPD frequently experience muscle atrophy/sarcopenia, decreased muscle strength and overall reduced muscular fitness. It is important to help your clients counter these physiological challenges with regular muscular training following the guidelines presented in Table 1.
- COPD is one of the top chronic conditions with the highest prevalence of falls, second only to osteoarthritis. Fall incidence in clients with COPD has been estimated to range between 25 and 46%. For this reason, balance training and fall prevention must be emphasized for all clients with COPD. However, because of their heightened risk for falls, it is important to be more conservative with balance-training exercises and progressions, and to provide more supervision and spotting.
Table 2. The Modified Borg Dyspnea Scale
The ACE Mover MethodTM in Action: Help Clients With COPD Exercise Safely
The ACE Mover Method was designed to empower clients to take a personalized journey toward achieving self-efficacy by fostering empathy, trust, communication and collaboration between the exercise professional or health coach and the client. Through actionable steps, the ACE Mover Method offers a way for exercise professionals and health coaches to help people move toward a better quality of life.
As a health and exercise professional, you recognize the importance of working closely with your clients, including those who have COPD, to design and implement safe and effective exercise programs. If you or your clients are uninformed or unprepared, exercising can bring unwelcome negative physiological responses, such as excessive breathlessness or chest discomfort and potentially even more severe health risks.
What is your client’s workload that elicits moderately severe dyspnea? What medications are they taking and do they interact with exercise responses? Does your client experience shortness of breath with any ADLs, and if so, which ones? The ACE Mover Method is a great approach to asking open-ended questions that help your clients better understand their condition and identify how they feel about their preparedness to safely exercise with COPD.
Some clients may have performed activities in the past that ended with excessive shortness of breath and, as a result, are anxious about engaging in future exercise programs for fear of repeating those untoward events. They may have experienced some close calls with falling and do not feel confident being in a gym. It is critical that you discuss any barriers that may be preventing your client from feeling comfortable with exercising with their COPD. For instance, they may feel unsure of how to safely balance the intensity and duration of exercise before it exceeds a threshold that causes symptoms.
Finally, collaborate and use your knowledge and what they have shared with you to come together and develop the best plan moving forward. Help educate your clients on how to identify their safe threshold for exercising. Collaborate with your clients to perform the talk test to identify their unique VT1 value and develop an exercise program that adheres to the intensity below VT1. Collaborate with your clients on physical settings where they will feel comfortable performing their various exercises.
Working with clients who have specific health challenges such as COPD can be challenging, yet highly gratifying. By utilizing the ACE Mover Method, you can set your clients up for success by helping them perform regular exercise safely and effectively while minimizing their COPD symptoms and disease progression.