By Lance C. Dalleck, PhD, Shawn M. Keeling, MSc, Ryan M. Weatherwax, MSc, and Joyce S. Ramos, PhD, with Daniel J. Green
While the value of physical activity and cardiorespiratory fitness are well established in terms of both health improvement and overall quality of life, it has been shown that not all individuals respond positively to regular aerobic exercise training following standardized guidelines. In other words, you may have clients who do everything you ask and exercise according to accepted exercise guidelines but still fail to experience the benefits of those efforts. Nothing could be more discouraging for trainer and client alike.
So, what’s missing?
Much research has been conducted comparing moderate-intensity continuous training (MICT)—think of 45 sweat-inducing minutes on the elliptical or treadmill—and high-intensity interval training (HIIT), which involves short, intense anaerobic exercise alternated with less-intense recovery periods (Ramos et al., 2017; Weston, Wisløff and Coombes, 2014; Tjønna et al., 2008).
The American Council on Exercise (ACE) decided to take things a step further and investigate whether an individualized program created by adhering to the ACE Integrated Fitness Training® (ACE IFT®) Model that combined MICT with HIIT would be more effective than the more traditional MICT-only approach at yielding important health and fitness benefits and deriving more consistent responsiveness. To find out, ACE enlisted the help of Lance Dalleck, PhD, and his team of researchers in the High Altitude Exercise Physiology Program at Western Colorado University.
The Study
The research team recruited 54 men and women aged 21 to 55 years, all of whom were nonsmokers, low-to-moderate risk and physically inactive, meaning they did not report participating in at least 30 minutes of moderate-intensity physical activity at three days per week for at least three months. In addition, none of the participants had evidence of cardiovascular, pulmonary and/or metabolic disease. All participants were asked to maintain their dietary habits and not perform additional exercise beyond that required for the study.
The participants were randomized into three groups. Group 1 was a non-exercise control group. Group 2 performed an individualized MICT plus HIIT program based on the ACE IFT Model (American Council on Exercise, 2014). Group 3 performed a standardized MICT program designed according to accepted industry guidelines (American College of Sports Medicine, 2018). The two training groups—referred to here as the MICT+HIIT group and the MICT-only group—performed a similar frequency and duration of exercise training
The Exercise Programs
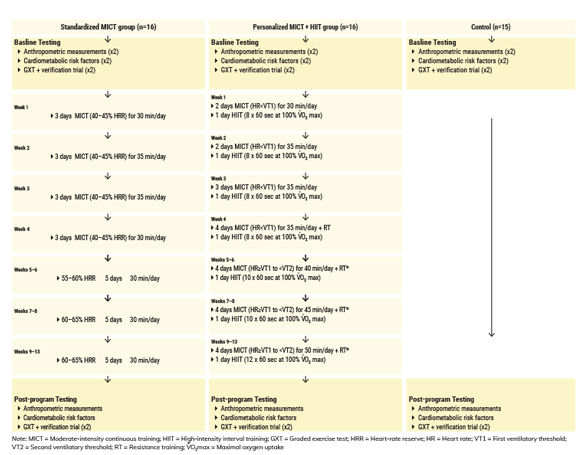
The MICT for both exercise groups was performed on a variety of aerobic modalities: arm, cycle and rowing ergometers; elliptical crosstrainer; and treadmill. Importantly, the method used to determine exercise intensity differed between the groups. For the MICT-only group, a standardized approach was used to program exercise intensity according to a percentage of heart-rate reserve (HRR). For the MICT+HIIT group, intensity was programmed based on each individual’s ventilatory threshold (VT). A target heart rate was established for members of both groups that coincided with either HRR or VT (Figure 1), which was then used to establish a specific exercise training intensity for each MICT session.
It is important to note that the programming for the HIIT sessions (MICT+HITT group only) was individualized as well. In addition to a five-minute warm-up and cool-down, at the outset each HIIT session consisted of eight 60-second interval bouts performed at the workload corresponding to 100% VO2max, separated by 150 seconds of activity recovery performed at a light intensity. This progressed as depicted in Figure 1.
Functional and resistance training began during week 4 of the program for both exercise groups and was performed three times per week for the remainder of the study. All sessions were supervised, and participants were monitored for adherence to the program, proper technique on all exercises and appropriate progression.
As with the cardiorespiratory workouts, the resistance-training program for the standardized MICT-only group was designed according to accepted industry guidelines (ACSM, 2018). The participants performed traditional single- and multijoint exercises using machines (e.g., shoulder press, lat pull-down and seated row). Participants completed two sets of 12 repetitions of each exercise, and resistance was progressed every two weeks by approximately 3 to 5% of total weight for the upper body and approximately 6 to 10% for the lower body.
The program for the MICT+HIIT group was designed according to ACE (2014) guidelines and consisted of multijoint/multiplanar exercises using free weights and machines that allowed for free motion during the exercise and unlimited range of motion (e.g., hip bridges, dumbbell squats and dumbbell bench press). Participants in this group also completed two sets of 12 repetitions. Intensity began at 50% of their five-repetition maximum (5-RM) and progressed by 5% increments every two weeks. For exercises that did not include a weighted resistance, the volume of each exercise was increased by approximately 5 to 10% every two weeks.
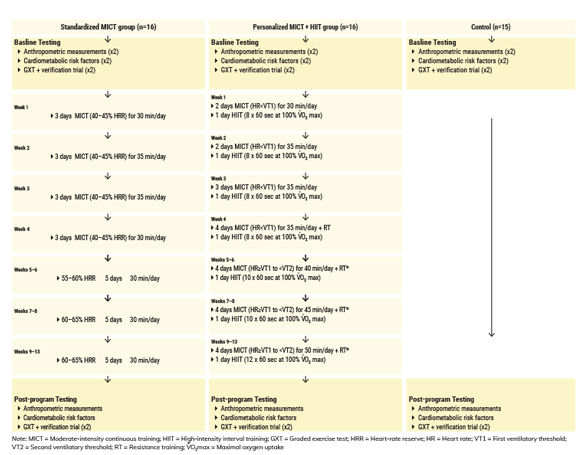
Figure 1
Experimental flow diagram and week-to-week exercise prescription for days/times of cardiorespiratory and resistance training.
The Assessments
Before and after the 13-week program, all participants underwent assessment of anthropometric measures, cardiometabolic risk factors and VO2max to develop personalized criteria for the identification of individual responders versus non-responders. Specifically, these assessments were as follows:
- Anthropometric measurements (weight, percent body fat and waist circumference)
- Fasting blood lipid and blood glucose
- Resting heart rate and resting blood pressure
- Metabolic syndrome z-score (MetS z-score; more on this below)
- Muscular fitness (5-RM)
- Maximal exercise testing and verification [maximal oxygen uptake (VO2max) and maximal heart rate (MHR)]*
- Ventilatory thresholds [first ventilatory threshold (VT1) and second ventilatory threshold (VT2)]
* Dr. Dalleck outlined the procedure for determining each participant’s “true VO2max” as follows: After a graded exercise test (GXT) to determine their VO2max, the participants rested for 20 minutes, then performed the test again for as long as they could at a workload 5% above what had been achieved during their GXT. VO2 was measured during this supramaximal bout. If it was within the margin of error, the individual’s VO2max was verified; if not, the procedure was repeated until the VO2max was confirmed. By adding this step to the process, the researchers helped ensure that any improvements in VO2max following the intervention were the result of a true training adaptation and not because of increased comfort with the GXT protocol.
The Results
At baseline, the three groups did not differ significantly in terms of physical and physiological characteristics. The exercise programs for both exercise groups were well-tolerated for the 32 of 36 participants who completed the study (the four who dropped out did so for reasons not related to the study). Overall adherence was excellent, as the MICT-only group completed 90% of their workouts and the MICT+HIIT group completed 91% of their workouts.
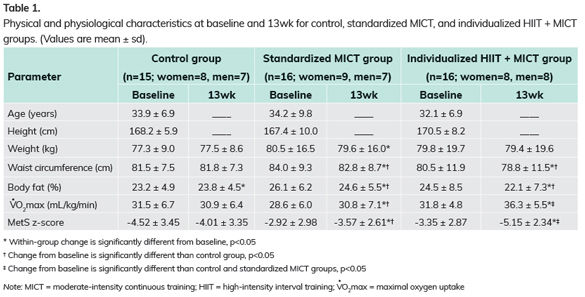
Table 1 presents the physical and physiological characteristics at baseline and after the 13-week training program. Percent body fat and waist circumference improved significantly for both exercise groups. However, changes in VO2max and MetS z-score were significantly more favorable in the MICT+HIIT group than in the MICT-only and control groups.
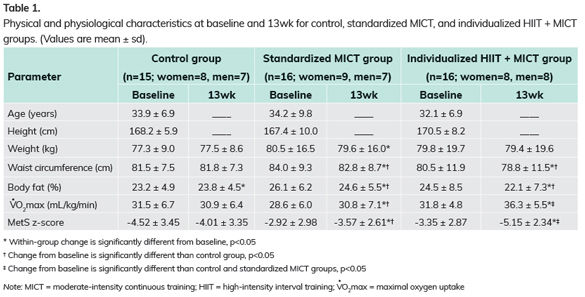
MetS z-score and Responders versus Non-responders
Traditionally, researchers looking into training responsiveness have used VO2max exclusively to quantify improvements in cardiorespiratory fitness, which provides a very narrow view. In contrast, the MetS z-score combines a number of cardiometabolic risk factor values into a single continuous score, including blood pressure, circumference measures, blood glucose, high-density lipoprotein and triglycerides (Malin et al., 2013). The primary benefits for inclusion of a continuous MetS z-score are twofold: (1) it acknowledges that there is a continuum to cardiometabolic risk within each individual and (2) it provides a more sensitive tool for assessing individualized training responsiveness following an exercise intervention.
“By broadening the assessment of training responsiveness using the MetS z-score, researchers are better able to capture the true benefits of an exercise program,” explains Dr. Dalleck.
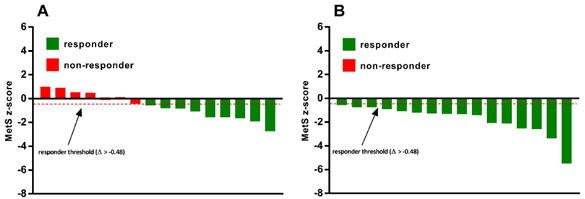
Of the subjects who participated in the individualized MICT+HIIT training in this study, 100% saw positive improvements in MetS z-score and were deemed “responders.” In the MICT-only group, only 56.25% saw a favorable change in MetS z-score and were categorized as responders. That leaves 43.75%, or seven out of 16 participants in the MICT-only group, who saw an undesirable change in their MetS z-score and were deemed non-responders to exercise training (Figure 2). The researchers found similar results when looking at responders versus non-responders in terms of changes in VO2max. The data on VO2max in isolation reveal that while 100% of the participants in the MICT+HIIT group were responders, only 68.75% of the MICT-only group responded positively to training.
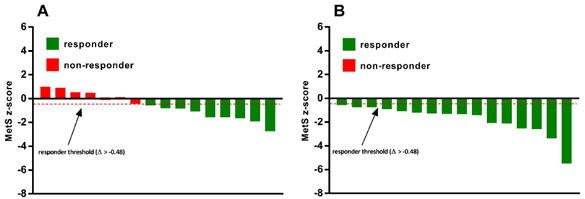
Figure 2
Inter-individual variability in MetS z-score responses to exercise training in the (A) standardized MICT-only group and (B) individualized MICT+HIIT group
The Bottom Line
The major findings of this study were twofold:
- A 13-week personalized exercise program that combined HIIT with threshold-based MICT elicited significantly greater improvements in both VO2max and MetS z-score when compared to standardized MICT alone.
- Individualized MICT+HIIT attenuated the inter-individual variation in VO2max and MetS z-score responses when compared to MICT alone, as evidenced by the significantly reduced incidence of training non-responders in the individualized program.
These results underscore the importance of a personalized and comprehensive approach to exercise programming in the effort to enhance training efficacy and limit training unresponsiveness.
One final note: When developing this study, the research team sought to create a program design that reflected what Dr. Dalleck calls “a real-world approach to personal training.” Much previous research has compared the benefits of MICT and HIIT training, but the truth is that for those clients who are fit enough to perform interval training as part of their workouts, the most effective approach—and the one used most often in the real world—combines the two. An essential factor in creating any program, no matter whether it involves MICT only or a combination of MICT and HIIT, is taking an individualized approach to programming intensity.
References
American College of Sports Medicine (2018). ACSM’s Guidelines for Exercise Testing and Prescription (10th ed.). Philadelphia: Wolters Kluwer.
American Council on Exercise (2014). ACE Personal Trainer Manual (5th ed.). San Diego: American Council on Exercise.
Malin, S.K. et al. (2013). Metformin modifies the exercise training effects on risk factors for cardiovascular disease in impaired glucose tolerant adults. Obesity, 21, 93-100.
Ramos, J.S. et al. (2017). Low-volume high-intensity interval training is sufficient to ameliorate the severity of metabolic syndrome. Metabolic Syndrome-related Disorders, 15, 319–328.
Tjønna, A.E. et al. (2008). Aerobic interval training versus continuous moderate exercise as a treatment for the metabolic syndrome: A pilot study. Circulation, 118, 346–354.
Weston, K.S., Wisløff, U. and Coombes, J.S. (2014). High-intensity interval training in patients with lifestyle-induced cardiometabolic disease: A systematic review and meta-analysis. British Journal of Sports Medicine, 48, 1227–1234.





 by
by