If you are a health coach or exercise professional, chances are you may have some clients who have prediabetes—and they may not even know it. The Centers for Disease Control and Prevention (CDC) note that more than one in three American adults have prediabetes, though 80% are unaware they have it, thus the nickname the “invisible epidemic” (CDC, 2020).
An individual is described as having prediabetes when he or she is experiencing insulin resistance or increased blood glucose levels that aren’t quite high enough for a diabetes diagnosis. A prediabetes diagnosis means that a person is on track for developing diabetes in the future, though it is reversible with lifestyle intervention.
While it’s alarming that such a large percentage of the population could be prediabetic without knowing it, the good news is that prediabetes can be reversed and type 2 diabetes can be prevented.
Who is at risk for having prediabetes?
The CDC lists the following as risk factors for prediabetes (CDC, 2020):
- Being 45 or older
- Having overweight
- Having a parent, brother or sister with type 2 diabetes
- Being physically active less than three times a week
- Ever having gestational diabetes (diabetes during pregnancy) or giving birth to a baby who weighed more than 9 pounds
- Having polycystic ovary syndrome
- Having glucose or A1C labs in prediabetic ranges (an A1C between 5.7 and 6.4% indicates prediabetes)
Who can help clients manage prediabetes?
Treatment for prediabetes involves implementing lifestyle interventions including increasing physical activity and improving nutritional habits. As a health and exercise professional, you are ideally positioned to assist this population. Helping clients set behavioral goals to improve nutrition and exercise habits can help to normalize labs and, in most cases, prevent the onset of type 2 diabetes.
Understanding Insulin Resistance
Insulin, a hormone that is made in the pancreas, is a key factor in the development of prediabetes and type 2 diabetes. When the body is healthy and functioning properly, insulin regulates blood glucose in the body by helping blood sugar enter into cells to be utilized for energy. However, when the body becomes insulin resistant, there is too much glucose in the blood stream and no way to use it—it’s resistant to the insulin the pancreas is pumping out.
Elevated blood glucose levels in combination with low high-density lipoprotein (HDL) cholesterol, high low-density lipoprotein (LDL) cholesterol, and elevated triglyceride levels may indicate insulin resistance. This combination can mean an increased risk of prediabetes or type 2 diabetes (CDC, 2019).
Interpreting Lab Values
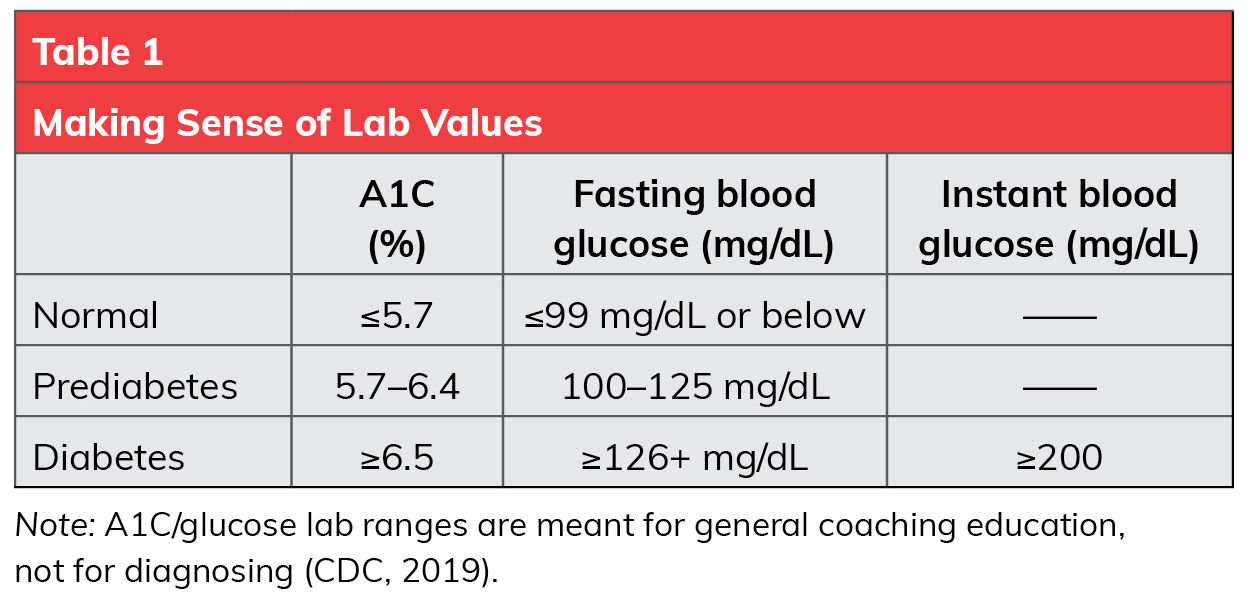
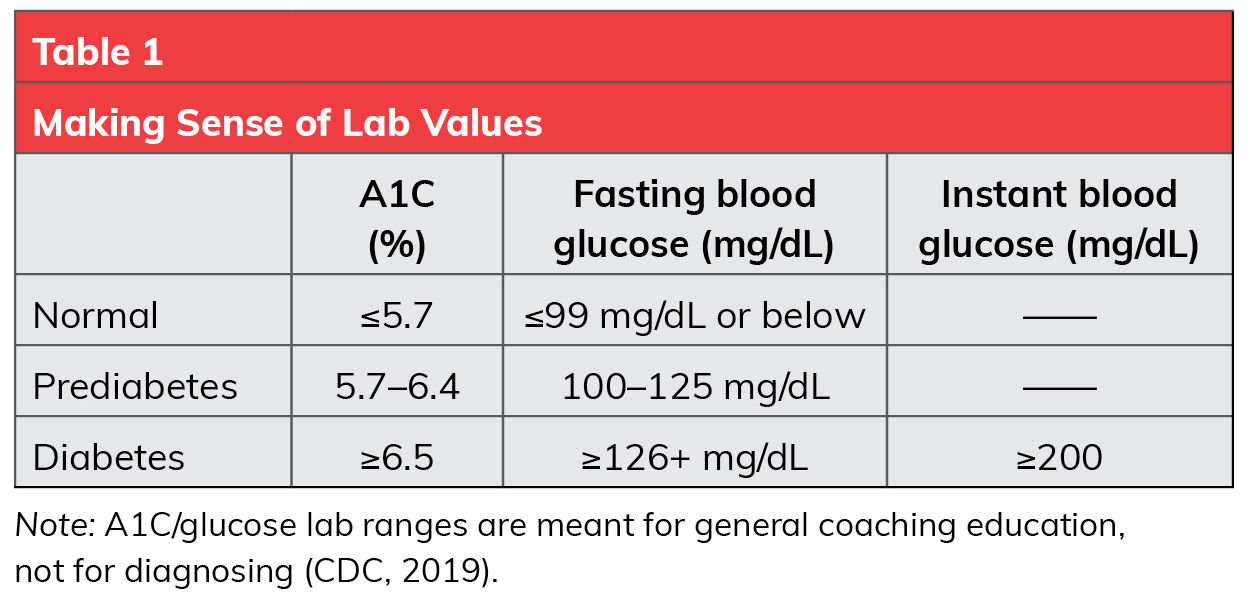
Three blood tests can be used to determine if a person has prediabetes; A1C, fasting blood glucose or an instant glucose test. A1C (also known as hemoglobin A1C or HA1C) is a measure of an individual’s average blood sugar over the past three months. The higher the A1C value, the greater the risk for developing diabetes (Table 1). The CDC recommends getting A1C checked for anyone over the age of 45, or for people younger than 45 who have overweight or one or more risk factors for prediabetes.
Fasting blood glucose measures blood sugar after not eating or drinking anything other than water overnight, while instant glucose testing measures the blood sugar on the spot.
Regardless of your client’s lab values, it’s important that he or she works closely with a physician or other healthcare provider to set a goal for A1C/glucose. As a health and exercise professional, you can support your clients in meeting behavioral or habit-based goals that serve to support healthy lab values. However, it is not within your scope of practice to diagnose or suggest a reduction in lab values without the support of a client’s medical provider.
Coaching Clients Who Have Prediabetes
When it comes to coaching clients with prediabetes, keep the following tips in mind:
- Demonstrate empathy for your clients. Given that many people with prediabetes are unaware they have it, and that there are generally no symptoms for prediabetes, it can be alarming for clients who receive a diagnosis. Any new diagnosis may be stressful and possibly trigger denial or worry about future health outcomes, so lending an empathetic ear to your clients can be a helpful first step. While a diagnosis of prediabetes may be distressing to a client, you can help clients gain perspective by noting that a prediabetes diagnosis is actually a chance to reverse their risk of developing diabetes. In many cases, with improved nutrition and increased physical activity, it’s entirely possible to get blood sugar levels back into normal ranges and prevent the onset of type 2 diabetes.
People who have family members who have been diagnosed with type 2 diabetes may be extra sensitive to receiving a prediabetes diagnosis. In this situation, it can be helpful to remind clients that family history does not guarantee they will get the disease. Furthermore, even in the case of family history, lifestyle changes can prevent chronic diseases and lead to improved health and quality of life.
Applied Coaching
Help your clients feel comfortable discussing their prediabetes diagnosis with you, urges Sarah Fergerson, a health coach and personal trainer based in Tulsa, Okla. “This topic can be sensitive to clients and talking about it may put them in a vulnerable place. I welcome their stories and guide them to understand their relationship with food,” she says. Fergerson also reminds clients about the impact their choices can have on their bodies and quality of life. “Prediabetes can be a great eye-opener. They still have time to make lifestyle changes to prevent the onset of type 2 diabetes. We discuss and find small habits they can work toward to create long-lasting changes.”
"Prediabetes can be a great eye-opener. They still have time to make lifestyle changes to prevent the onset of type 2 diabetes."
2. Manage blood sugar with exercise. Physical activity allows glucose in the body to be more readily utilized. The latest edition of the Physical Activity Guidelines for Americans recommends that adults participate in at least 150 minutes of moderate-intensity physical activity per week. According to the guidelines, “adults who regularly engage in aerobic activity of at least moderate intensity have a significantly lower risk of developing type 2 diabetes than do inactive adults. These benefits begin to accrue at levels of physical activity below the key guideline of 150 to 300 minutes a week, and additional amounts of moderate- or vigorous-intensity physical activity seem to lower risk even further.” Even more good news: “Insulin sensitivity can be improved with just a single bout of physical activity” (U.S. Department of Health and Human Services, 2018). For sedentary clients, slowly increasing physical activity levels and intensity can be beneficial, rather than immediately going from 0 to 150 minutes per week.
Applied Coaching: Helping clients to make gradual changes can begin to reduce the risk for type 2 diabetes. Use motivational interviewing to help clients determine what activities they are most interested in doing. Understanding your clients’ interests—if they prefer indoor or outdoor activity, for example, or would rather exercise alone than with other people—can help identify the activities that may be a good fit for them. There are endless ways to engage in low-impact physical activity including walking, biking, hiking, attending gym classes, weightlifting, indoor cycling, dancing, etc. It is important to realize, however, that clients are more likely to adhere to a new physical activity when they come up with the plan (as opposed to following the directives of a coach or trainer). Framing the plan as a no-fail experiment and emphasizing that there is no consequence if they don’t like the activity they chose can take the stress out of trying something new.
3. Manage blood sugar with nutrition by increasing fiber intake. Increasing fiber intake while also balancing protein, fat and carbohydrate consumption can help clients begin to improve their overall health and better manage blood sugar levels. Focusing on whole grains and foods with fiber and protein can help keep blood sugar in check and avoid spikes; conversely, foods or drinks high in sugar can increase blood sugar in the body. A 2015 study highlighted the benefits of consuming fiber-rich foods such as beans, legumes, fruits, vegetables and whole grains in the prevention of diabetes. Researchers concluded that adult women should consume a minimum of 25 grams of fiber per day, while men should aim for 38 grams per day (Dahl and Stewart, 2015).
Applied Coaching: Take the time to educate clients about insulin resistance and high blood sugar. “I find explaining high blood sugar, insulin resistance and insulin sensitivity to clients helps open their eyes,” explains Sarah Stout, MS, a health coach who has experienced her own journey of losing weight and normalizing blood sugar levels. “I try to explain what insulin does and why it's important to avoid blood sugar spikes as well as why it's important to eat complex carbs for sustained energy.” While you don’t want to get overly technical, knowing what is happening in the body can help clients understand the consequences of poor choices and the benefits of healthier habits.
Case Study
Now let’s put this knowledge into practice. A 39-year-old woman comes to you for coaching. She admits to frequently skipping meals because she’s busy caring for her kids, which means she often consumes sugary foods in the evening after dinner. She is physically inactive, has an elevated body mass index (BMI), borderline high glucose lab levels, a low HDL cholesterol level and elevated triglycerides. She was recently given a prediabetes diagnosis, which was a shock to her, but she’s hoping to change course, improve her health and avoid developing type 2 diabetes.
As a health coach, here are some recommended steps you might take:
- Utilize motivational interviewing to assess your client’s readiness to change. Clients may hire a coach as a result of a diagnosis even if they aren’t quite ready to begin making habit changes. This is particularly true if a client assumes he or she will have to make many changes at once or need to give up favorite foods. Exhibiting genuine curiosity about a client's underlying desires for change and thoughts about his or her diagnosis, as well as utilizing motivational interviewing techniques, can help you and your client build rapport and collaborate on a plan.
Here are some sample talking points you might employ:
- Tell me more about what led you to hiring a coach. What was going through your mind when you received that diagnosis? That must have been stressful for you. Are you open to begin making some changes with nutrition or exercise?
- Receiving a diagnosis like prediabetes can feel overwhelming. The good news is that making some changes with your nutrition and exercise habits (even starting with small changes) can minimize your risk of developing diabetes. Is there anything that comes to mind that you think would be most helpful to work on first? How would you like your health to be different six months or one year from now?
- After discussing the client’s underlying desires for change and potential long-term goals, help her identify the habits that lead to managing prediabetes and preventing type 2 diabetes. For example, she might start improving her nutrition by increasing fruit and vegetable intake, consuming fewer sugary drinks, or limiting dessert to two days per week. If the client does not currently exercise, it may be helpful to first identify the types of exercise that might interest her, how much time she can dedicate to exercise, etc. Discuss which type of goal the client would like to focus on first.
- After setting a short-term (one- to two-week) goal, help the client identify potential barriers to achieving her goal. Some common examples include lack of time/busy schedule, lack of family support, etc. Discuss a plan for managing each barrier, such as including shorter workouts, meal prepping or buying pre-chopped vegetables, coming up with discussion points for talking to a partner/family/friend group about her desire or motivation for change, inviting the partner to participate in a workout or having scheduled workouts with the coach.
- Utilize short-term goals and frequent check-ins. Weekly or bi-weekly goal check-ins (in person, through text or via video chat) offers clients ongoing accountability and the ability to quickly tweak goals that aren’t working (e.g., the client finds that working out four days per week isn’t doable right now). In addition to encouraging the client to participate in ongoing goal adjustments, frequent check-ins can prevent her from getting discouraged or frustrated if a goal isn't working for her, or if the goal becomes too easy.
- Don’t forget to check in on long-term goals as well. Having lab checks or weigh-ins on a less frequent basis can provide quantitative data to consider and help you and your client know if the plan is working or if additional adjustments are necessary.
Remember, even if a client has several risk factors, it is not your job as a health and exercise professional to diagnose or suggest a client has prediabetes. Rather, focus on guiding your clients toward improved habits that will reduce their risk of developing chronic diseases such as type 2 diabetes.
References
Centers for Disease Control and Prevention (2020). Prediabetes−Your Chance to Prevent Type 2 Diabetes.
Centers for Disease Control and Prevention (2019). Diabetes Basics: Getting Tested.
Dahl, W.J. and Stewart, M. L. (2015). Position of the Academy of Nutrition and Dietetics: Health Implications of Dietary Fiber. Journal of the Academy of Nutrition and Dietetics, 115, 11, 1861–1870.
U.S. Department of Health and Human Services (2018). Physical Activity Guidelines for Americans, 2nd edition. Washington, D.C.: U.S. Department of Health and Human Services.





 by
by