When it comes to getting enough daily physical activity, Americans, as a whole, could do better. After all, more than a quarter of adults in the United States don’t participate in any leisure time physical activity, according to 2020 data from the National Health Interview Survey. Not only is physical inactivity associated with numerous health concerns, including obesity, hypertension, type 2 diabetes and atherosclerotic cardiovascular disease, it contributes annually to $117 billion in annual healthcare costs and 10% of premature deaths.
Currently, adults age 65 or older are the least physically active of all age groups. They also hold the distinction of being part of the fastest growing demographic group. In fact, the number of Americans age 65 and older currently stands around 56 million, or more than 16% of the total population. These numbers mirror similar trends in other developing countries, particularly in Europe.
What does this mean for you as a health and exercise professional? As more Americans cross the 65-year mark, your chances of working with clientele other than apparently healthy adults will undoubtedly increase. Older adults often deal with challenges such as balance impairments, osteopenia, sarcopenia and other health-related disorders, all of which require unique modifications to their exercise programs. Read on to learn 10 key exercise-programming tips for creating effective exercise programs for your older adult clients.
The Physiology of Aging
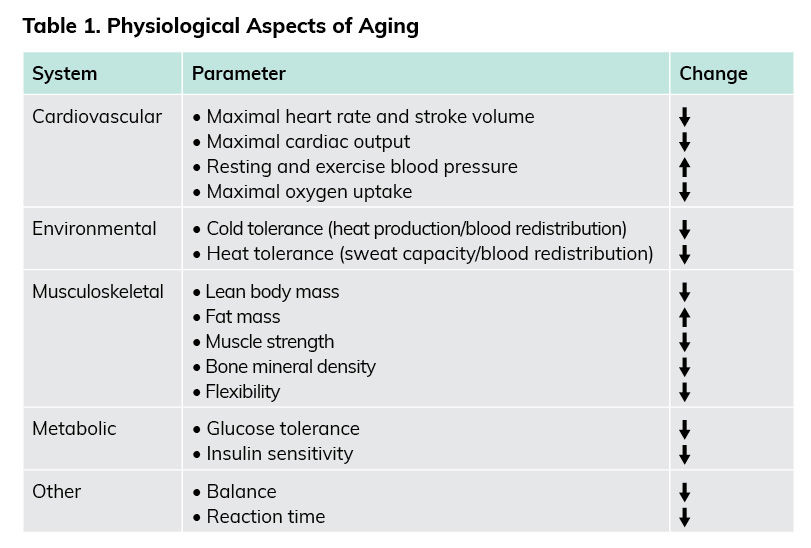
Older adults are typically defined as individuals who are age 65 or older. Others who might fit into this category include adults aged 50 to 64 years who have clinically significant chronic conditions and/or functional limitations that impact movement ability, fitness or physical activity. Despite these age ranges, you should not erroneously assume that chronological age equates to physiological or functional age. Indeed, persons of similar ages can differ remarkably in functional capacity, which in turn affects how these individuals respond to exercise. Although it is inevitable that physiological function will decline with age, the rate and magnitude of change is dependent on a complex interaction of genetics, individual health, presence of disease or injury, and exercise history. Safe and effective exercise programming for older adults requires that you have knowledge of the effects of aging on physiological function at rest and throughout the exercise intensity spectrum. A list of key physiological aspects of aging is presented in Table 1. Being aware of the physiological aspects of aging will help you and your clients establish realistic program goals.
Previously sedentary older adults who start an exercise program can expect improvements in numerous health parameters. However, due to the natural decline in function associated with aging, you should also view maintaining function as a successful exercise-program outcome. For example, previous research suggests that people experience, on average, a 6 to 10% decrease in cardiorespiratory fitness per decade after the age of 40. If you work with a client for several years and observe no change in their cardiorespiratory fitness level over that timeframe, you have, in fact, designed and implemented an effective program because the inevitable decline in physiological function, in this case cardiorespiratory fitness, has been delayed.
When designing exercise programs for older adults, keep these three overarching goals in mind:
- Prevent or delay the progression of chronic diseases
- Maintain or enhance cardiorespiratory fitness levels
- Prevent functional limitations and disabilities
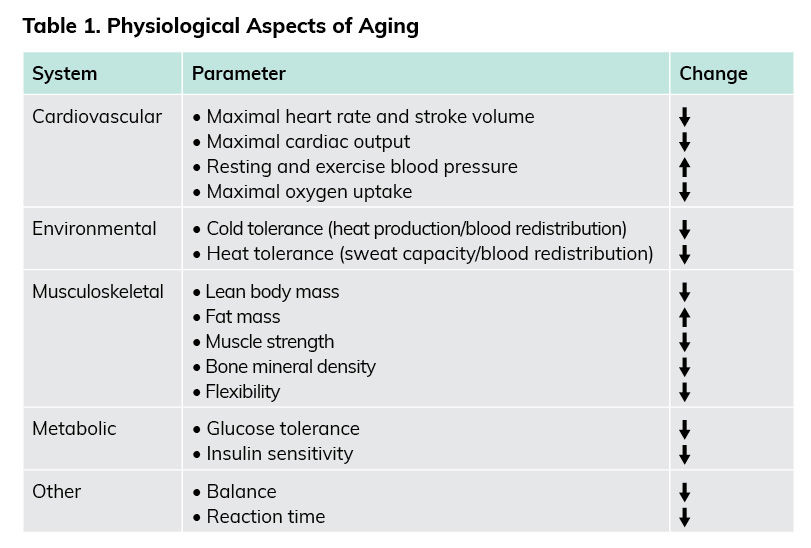
*adapted from American College of Sports Medicine, 2021
10 Key Exercise Programming Tips for Older Adults
Keeping these goals in mind, use the following 10 tips to guide your programming decisions for your older-adult clients.
1. Incorporate Regular Balance Training
Improving proprioception should be a primary goal when designing exercise programs for older adults. Regularly incorporating flexibility, balance and lumbar strength training into the exercise design can increase adherence and quality of life. Loss of mobility and balance results in approximately 2.5 million older adults being treated in emergency departments each year for broken bones or head injuries. After the age of 30, adults lose, on average, 3 to 8% of their muscle mass per decade, which results in decreased muscular strength and power. Functional balance training is essential for older adults to ensure their ability to continue important activities of daily living, such as bathing, getting dressed and stair climbing.
The ability to divide attention between a proprioceptive and a cognitive task is known as dual tasking, which is common in everyday life. Balance-training programs for the older adult population should focus on functional and progressive tasks of daily living. The aim of a balance-training program is to improve gait and balance deficits in older adults and reduce the fear of falling and to increase self-esteem and physical-activity levels. Some examples of different training programs include dual- and multitask exercises related to falling, such as spelling words while doing balance exercises, standing core exercises and TRX suspension training. Check out this earlier article for more information on balance programing.
2. Understand Common Response Interactions Between Medication and Exercise
In addition to exercise, millions of Americans currently take prescribed medications to manage various chronic conditions, such as high cholesterol, hypertension, type 2 diabetes and cardiovascular disease. Therefore, it is critical that you understand the interaction of certain medications with the exercise response.
The five most common medications prescribed to older adults are beta blockers, ACE inhibitors, diuretics, antihyperlipidemics and antidiabetics, with the percentage of American adults taking these medications increasing at age 65 and older. Beta blockers elicit lower heart rate and blood pressure responses to a given exercise workload. Individuals on ACE inhibitors and diuretics have both lower resting and exercise blood pressure values. A primary concern for individuals taking ACE inhibitors and diuretics is that the combination of the reduction in blood pressure from both of these categories of medications, combined with a naturally occurring post-exercise hypotension, can result in excessive reductions in blood pressure. Individuals who take statins should take caution with intense exercise due to the association between the drug and exertional rhabdomyolysis. Finally, oral hypoglycemics influence the transport of glucose from the blood into skeletal muscle and can increase the potential risk for exercise-induced hypoglycemia. This earlier article includes additional information on how common medications may affect how an individual responds to exercise.
3. Consider Maintenance and Compliance to Be Key Program Outcomes
Research suggests that as many as 80% of those who begin an exercise program will not adhere to the program for more than six months, even though exercise adherence is a key factor in the prevention and management of chronic diseases, risk factors and functional disabilities associated with aging. While this figure is disturbing, it underscores the importance of encouraging compliance among your clients (of every age) to achieve favorable outcomes (i.e., lower incidence of hypertension and diabetes, prevention or delay of osteoporosis, lower triglycerides and cholesterol, a decrease of obesity and musculoskeletal disorders, and fewer depressive symptoms and stress). To encourage adherence, the programs you design for your older adult clients should emphasize activities they enjoy, which might include walking in groups on outdoor trails, walking on a treadmill or around neighborhoods, resistance training focused on functionality of movement, aquatic exercise, yoga, tai chi and balance exercises.
4. Remember, Mental Health Is Just as Important as Physical Health
Not only is regular exercise beneficial in attenuating the aforementioned decline in physiological characteristics associated with aging, exercise also aids in the maintenance and improvement in psychological well-being. Research suggests that higher cardiorespiratory and muscular fitness are associated with a reduced risk of developing common mental disorders, including depression and anxiety. With the associated psychological and physiological improvements to mental health, it is important to pay considerable attention to psychological well-being during intake interviews and throughout exercise progression and note any changes that occur. If you are concerned about the mental health of your older adult client, this list of mental health resources for older adults could be helpful.
5. Use the Talk Test to Monitor Aerobic Exercise Intensity
A percentage of maximal heart rate is generally considered a viable method to quantify aerobic exercise intensity. However, as individuals age, they can differ greatly in their body’s physiological response to exercise (i.e., heart-rate response). This is because aging is not a uniform process. For this reason, the 0-to-10 rating of perceived exertion (RPE) scale is often recommended for use with older adults to classify aerobic exercise intensity, with a rating of 3 to 4 for moderate intensity, 5 to 6 for vigorous intensity and 7 to 10 for near-maximal intensity. However, the desired level of exercise intensity may not be achieved while using the RPE method due to the subjectivity of the measurement. An alternative measure of aerobic intensity is the talk test, which is a practical way to identify ventilatory thresholds. The talk test helps to individualize aerobic exercise intensity recommendations, and has been shown to be valid on both the treadmill and bike.
To implement the talk test, pay close attention to the ability of your client to talk as they are exercising. As exercise intensity increases, talking will become more difficult as the client nears the first ventilatory threshold. Eventually, talking will become very uncomfortable the closer the client gets to the second ventilatory threshold. Beyond the second ventilatory threshold, clients will have great difficulty talking. To anchor the talk test to the RPE scale, a 5 is associated with talking with groups of four to five words between breaths and a 7 is equal to the participant being unable to talk and keep the same pace. Therefore, the talk test serves as a practical way to establish and monitor cardiorespiratory exercise intensity in older adults.
6. Use RPE (Not %1-RM) to Quantify Resistance Training Intensity
The aging process generally includes a reduction in muscle mass, which leads to declines in muscular strength, power, endurance, balance and mobility. These negative effects of aging can be attenuated by a progressive resistance-training program, with results of 9% to more than 100% improvements in muscular strength. Traditionally, when recommending resistance-training exercise, a percentage of one-repetition maximum (1-RM) is used to quantify intensity. However, performing maximal work (true 1-RM or equating max from maximal repetitions) may be contraindicated due to many older adults falling into the moderate- and high-risk categories for health risk stratification.
Therefore, an alternative approach using RPE is warranted when working with older adults. To maximize a client’s strength gains, a total of eight to 10 resistance-training exercises on two or more non-consecutive days, with 10 to 15 repetitions per set, are needed. The overall resistance should account for a moderate-to-vigorous RPE of 3 to 4 and 5 to 6, respectively, when using a 0-to-10 scale. By implementing the RPE method, the risk of performing maximal work is removed.
7. Incorporate Eccentric Exercises Into the Training Program
The use of eccentric exercise (which focuses on the lengthening phase of a muscle action while force is being applied) has drawn considerable interest for improving overall strength. Eccentric exercise has properties of high-force production with an overall low energy cost, making this exercise modality appealing for use with older adults. Indeed, research suggests that performing two sets of 10 repetitions of eccentric exercises over four months can elicit considerable improvements in strength. However, it should also be noted that a variety of eccentric resistance-training protocols have been utilized in past research studies, and there is currently no single “best set protocol” for use with older adults. As with many training variables, gradually progressing eccentric resistance training is essential to help avoid muscle damage.
8. Integrate HIIT Into the Older Adult Exercise Routine
High-intensity interval training (HIIT) involves alternating brief bouts (30 seconds to five minutes) of higher-intensity sessions with either rest or lower-intensity workloads throughout an exercise routine. Numerous studies have demonstrated that HIIT may be a more time-efficient approach than continuous moderate exercise for achieving specific health benefits in the older adult population. For example, a study by Ann-Marie Knowles and her colleagues had participants perform HIIT sessions on a cycle ergometer once every five days for six weeks (nine total HIIT sessions), with each session consisting of six 30-second sprints at workloads equating to 90 to 100% maximal oxygen uptake (VO2max). The 30-second interval bouts were separated by three minutes of active recovery that was comprised of low workloads (0 to 50 Watts) performed at a self-selected speed. Overall, the research to date on the effectiveness of HIIT in older adults shows that it improves quality of life, motivation to exercise and levels of cardiorespiratory fitness.
One of the most important things to remember when integrating HIIT into the exercise routines of older-adult clients is to provide additional time for recovery. Critically, the Knowles study clearly demonstrated that five days of recovery is required between HIIT sessions for older adults.
9. Encourage Flexibility Training Performed at the Correct Time
Flexibility, which is an essential component of physical fitness, decreases with age and physical inactivity. Poor flexibility, coupled with decreased musculoskeletal strength, is associated with a diminished ability to perform activities of daily living. Consequently, the beneficial effect of static stretching on the achievement and maintenance of flexibility should not be overlooked.
The guidelines for designing flexibility programs for older adults are similar to those for younger individuals. Over the past two decades, there has been considerable scientific inquiry on the topic of pre-exercise stretching and performance/risk of injury. Collectively, present research findings suggest that there are no ergogenic benefits, and potentially detrimental effects (decreased muscular strength and endurance, impaired balance and diminished reaction time), to incorporating static stretching exercises into a warm-up routine. These findings are consistent among different populations and research designs, including untrained and trained individuals, recreational and competitive athletes, men and women, and with or without an aerobic warm-up. Accordingly, be mindful of this robust evidence when designing programs for older adult clientele and ensure that flexibility training is included after the cardiorespiratory, resistance and balance-training components.
10. Be Mindful of Special Considerations for Programming for Older Clients with Comorbidities
An estimated four out of five individuals aged 65 years or older are living with at least one chronic health problem, and half of these adults are living with two chronic conditions. As a health and exercise professional, it is increasingly likely that you will work with clients who have multiple chronic conditions. However, numerous health organizations, including the American Council on Exercise, list sedentary lifestyle as a modifiable risk factor for many chronic health conditions. Accordingly, exercise is a common therapeutic intervention strategy for individuals with multiple chronic conditions. Here are several tips for designing programs for older clients who have one or more chronic health condition:
- Individuals with multiple chronic conditions may require medical clearance before participating in an exercise program, depending on the presence of symptoms and current levels of physical activity.
- You and your client should ask the client’s medical team about any specific limitations to be aware of when designing the exercise program (e.g., specific exercises to avoid).
- One strategy to employ when working with clients who have chronic health conditions is to design the overall exercise program around the condition that poses the greatest risk to the health of the individual.
- Individuals with multiple chronic conditions may experience symptoms that fluctuate significantly from day to day in terms of severity (e.g., low-back pain, osteoarthritis, fibromyalgia). You must be prepared to accommodate an ever-changing chronic-condition landscape with these clients and constantly adjust the session to best serve your clients on any given day.
Summary
As health and exercise professionals, your work with older adults will undoubtedly be deeply gratifying. By promoting regular exercise, you can help your clients attenuate the aging process while also reaping numerous health benefits. More importantly, your clients will maintain independence and the ability to perform activities of daily living for longer and enjoy an overall greater quality of life.
Expand Your Knowledge
The NEW and IMPROVED ACE Senior Fitness Specialist Program teaches you how to safely and effectively help senior clients maintain vibrancy through health and fitness. You’ll discover a holistic approach to both body and brain health, combining rapport-building, behavior change, exercise programming, nutrition and cognitive health. Most older adults are impacted by some type of age-related chronic illness, injury or cognitive decline, so this specialized expertise will help increase your value and client pool.
The U.S. Census Bureau predicts that 83.7 million people aged 65 and older will be living in the United States by 2050, creating a high demand for trained professionals to help older adults focus on their health and fitness. From strength training and motivation to body and brain improvement, the Essentials for Training Older Adults – Course Bundle dives deep into improving your senior clients’ fitness and quality of life.
Based on the research series “ACE Health and Wellness Reports,” this practical course outlines the role that physical activity plays in delaying age-related declines in functional ability as well as in the prevention and management of chronic health conditions common to older adults, such as osteoporosis, arthritis, depression, and cardiovascular disease and its risk factors. You’ll learn how to plan, prepare, implement and make modifications to older clients’ exercise and wellness programs to meet their individual needs and goals so that they can achieve and maintain vibrancy, vitality and vigor as they age.





 by
by