High blood pressure (a.k.a. hypertension) happens when the force of blood pushing against the walls of blood vessels is too high, and can lead to serious health problems such as heart attack and stroke. In fact, hypertension is a leading risk factor of cardiovascular disease. Worldwide, an estimated one in four adults—more than 1.3 billion people—are believed to have hypertension. In the United States, nearly half of all adults—nearly 120 million people—have hypertension. Clearly, the chances that you will be working with clients who have been diagnosed with hypertension are quite high, but here’s the good news: exercise is a well-known antidote to hypertension with both acute and chronic benefits, with research showing an inverse relationship between exercise and blood pressure levels. This article outlines strategies for helping your clients with hypertension perform exercise safely and effectively. We’ll also explore other lifestyle modifications that can positively influence blood pressure.
Common Medication–exercise Response Interactions and Exercise Program Modifications
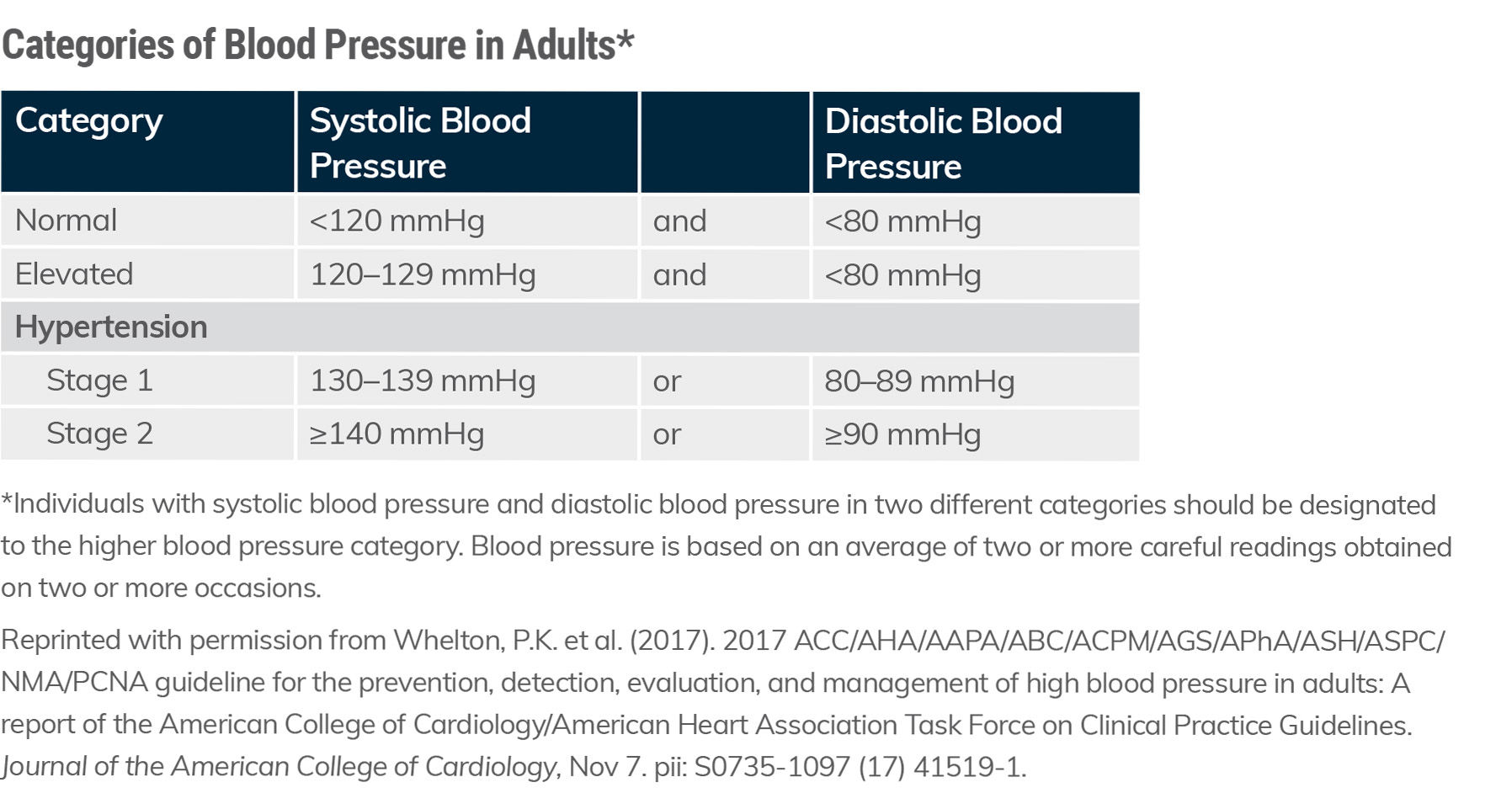
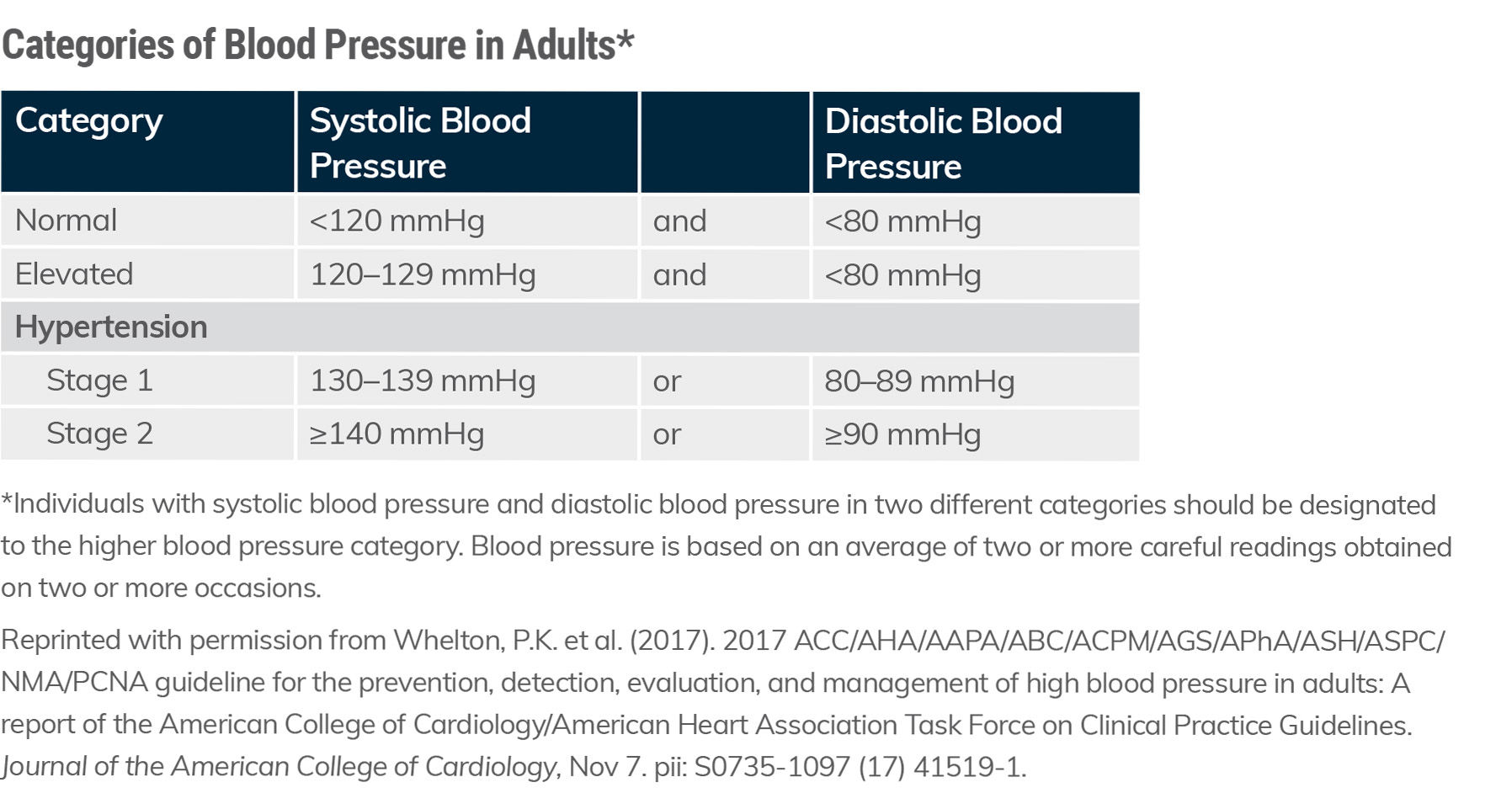
The different categories of blood pressure in adults are presented in Table 1. The medical management of hypertension may consist of a broad range of medications. As a health and exercise professional, it is critical to understand the interaction of certain medications with the exercise response and how the exercise program might need to be adjusted. Indeed, some of the most common medications prescribed to Americans are those likely to be prescribed to clients with hypertension, including ACE inhibitors. In fact, 10-20% of American adults are prescribed an ACE inhibitor medication.
Table 1. Categories of Blood Pressure in Adults
Mechanism of Action
An ACE inhibitor (or angiotensin-converting-enzyme inhibitor) is a medication primarily used for the treatment of hypertension. Common ACE inhibitors include captopril, enalapril and lisinopril. ACE inhibitors reduce the activity of the complex renin-angiotensin-aldosterone system. Simply put, ACE inhibitors block the conversion of angiotensin I to angiotensin II primarily in the lungs. The molecule angiotensin II is a potent vasoconstrictor of blood vessels. Therefore, reduced production of this molecule results in relaxation of the blood vessels and lower blood-pressure values.
Fast Facts About Hypertension
- Most people with hypertension (90 to 95%) have primary hypertension (previously called essential hypertension), which is multifactorial and doesn’t have one distinct cause. A distinct cause of hypertension would be a medical condition or a medication side effect. Primary hypertension can be caused by an interaction between unhealthy habits (e.g., sedentary lifestyle, sleep issues, poor diet and alcohol use disorder) and certain circumstances, such as age and having a family history of high blood pressure.
- In the other 5 to 10%, hypertension is the result of an identifiable cause, such as kidney disease, and is designated secondary hypertension.
- The overall prevalence of hypertension (blood pressure >130/80 mmHg) is 46% in American adults, though estimates vary by race and ethnicity. An estimated 44% of Hispanics, 45% of Asians, 47% of Caucasians and 59% of African Americans have blood pressure levels above that threshold or report using antihypertensive medication.
- The prevalence of hypertension increases with age, such that 50% of people aged 45 to 54 years and 79% of those aged 75 years or older are affected. According to one study, hypertension is responsible for the second highest number of overall deaths among American adults.
Interactions Between Medication and Exercise Response
Individuals on ACE inhibitor medication have both lower resting and exercise blood-pressure values. However, it is the interaction between ACE inhibitors and the post-exercise blood-pressure response that requires your additional attention. An acute beneficial response to exercise is a phenomenon known as post-exercise hypotension, whereby systolic blood pressure values can be reduced by 5 to 7 mmHg for up to 22 hours after the conclusion of exercise. This occurs due to a persistent, but transient, relaxation of the blood vessels. The concern for individuals taking ACE inhibitors is that the combination of the reduction in blood pressure from the medication coupled with the naturally occurring post-exercise hypotension can result in excessive reductions in blood pressure. This can lead to untoward events such as dizziness and, in rare instances, syncope (i.e., temporary loss of consciousness).
It is critical that clients who take ACE inhibitors consistently adhere to a gradual cool-down after each and every exercise session. One of the classic benefits of a cool-down is enhanced venous return and the prevention of blood pooling in the skeletal muscle. A gradual cool-down of five to 10 minutes of light cardiorespiratory exercise at the conclusion of the overall workout permits the body to return to homeostasis and prevents excessive reductions in blood pressure.
Diuretics and beta blockers are two other medications that are commonly prescribed to individuals with hypertension. Much like ACE inhibitors, diuretics can cause an individual to have both lower resting and exercise blood-pressure values. The combination of the reduction in blood pressure from both categories of medications, combined with a naturally occurring post-exercise hypotension, can result in excessive reductions in blood pressure. An easy solution is to add a two- to three-minute cool-down to every cardiorespiratory exercise within the overall workout.
Beta blockers function by preventing the binding of epinephrine to receptors in the heart. This results in decreases in both resting and exercise heart-rate and blood-pressure values. The fact that beta blockers attenuate the heart-rate response to exercise means traditional methods for establishing target heart rate (e.g., peak heart-rate method or heart-rate reserve method) are likely to be invalid. Therefore, the most important program design modification for clients taking a beta blocker is to use an alternative method for setting target intensity. The talk test is an excellent option.
The intent of this section is not to be exhaustive in its scope. Rather, it’s to highlight important considerations for medication–exercise response interactions and subsequent exercise program modifications that you must be aware of when working with clients who have hypertension. Take the time to collaborate with your client’s multidisciplinary team of medical providers and familiarize yourself with any other relevant medications and considerations for overall exercise programming.
Exercise Programming for Clients Who Have Hypertension
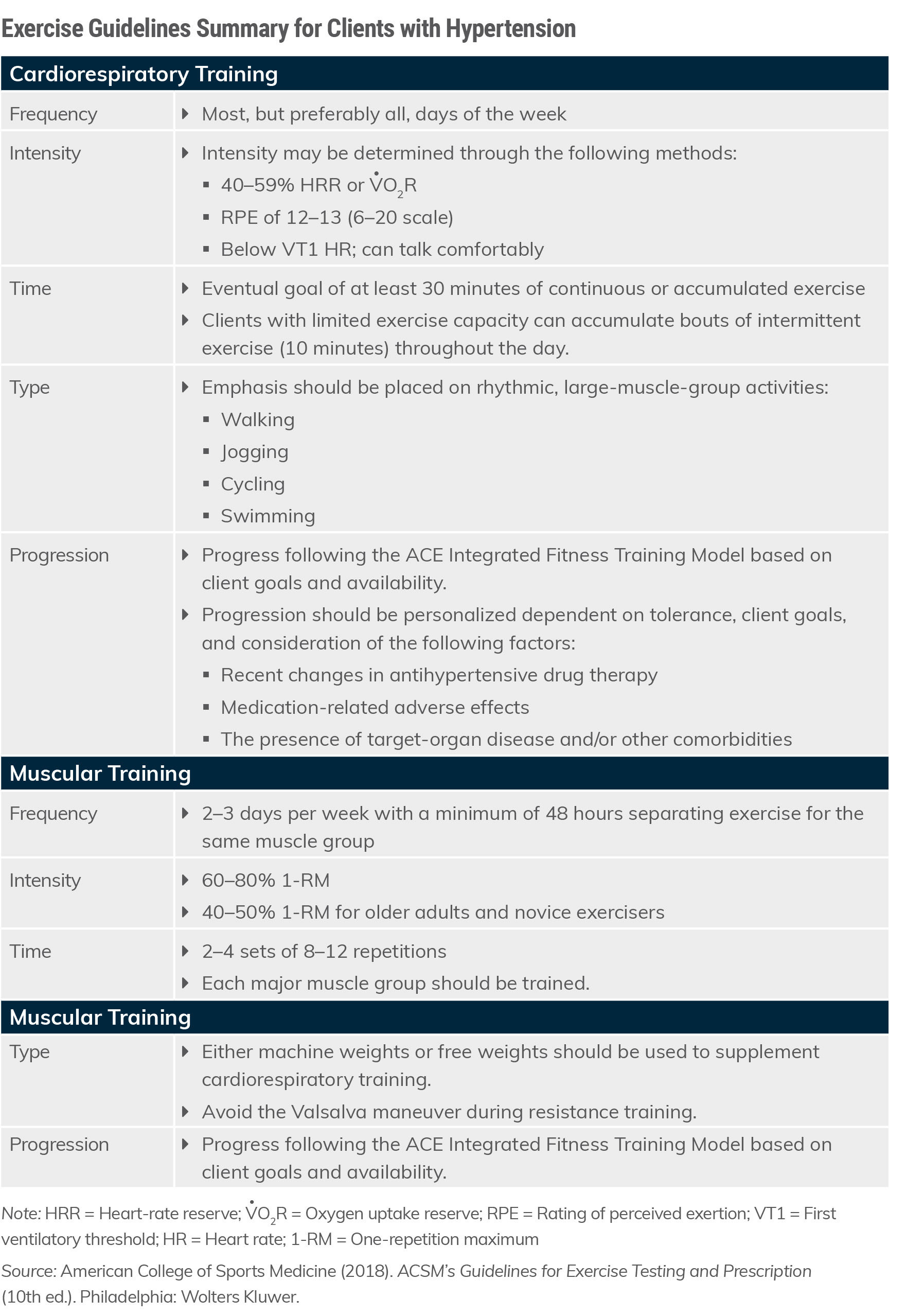
As mentioned earlier, a single, acute bout of moderate-intensity exercise can lower systolic blood pressure by 5 to 7 mmHg for up to 22 hours after the completion of the exercise session. Interestingly, the chronic benefits from exercise training in terms of blood-pressure reduction are less pronounced, with the literature reporting a decrease of 3 mmHg and 2 mmHg in systolic and diastolic blood pressure, respectively, after one to six months of cardiorespiratory training. Muscular training has also been shown to reduce blood pressure; however, the blood-pressure change is not as pronounced as it is following cardiorespiratory training. Combined cardiorespiratory and muscular training appears to produce a similar reduction in post-exercise blood pressure as cardiorespiratory training alone.
The volume of regular cardiorespiratory exercise that has consistently been shown to reduce systolic blood pressure and diastolic blood pressure is 150 minutes per week or more, with the greatest reductions occurring in individuals with hypertension. This volume of activity is consistent with the Physical Activity Guidelines for Americans and recommendations by the American College of Sports Medicine. Individuals with elevated blood pressure and those with hypertension should participate in regular exercise of moderate intensity for 30 minutes or more at least five, if not more, days of the week. Cardiorespiratory activities such as walking, cycling, elliptical cross training, stairclimbing and swimming are excellent modes of exercise and should be supplemented with muscular training at least two times per week whenever possible.
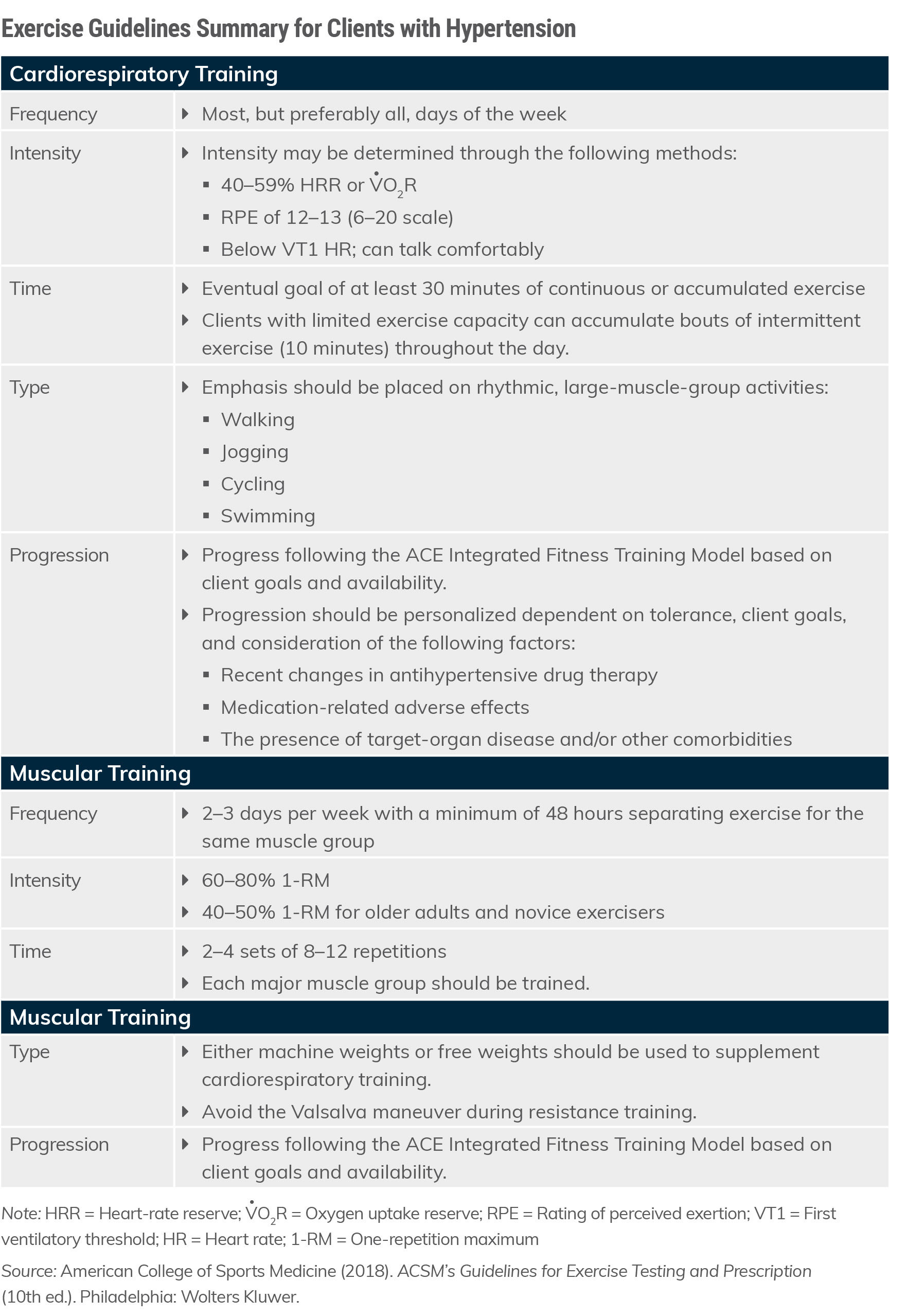
Table 2 presents exercise guidelines for cardiorespiratory and muscular training to follow when designing programs for clients who have hypertension.
Table 2. Exercise Guidelines Summary for Clients Who Have Hypertension
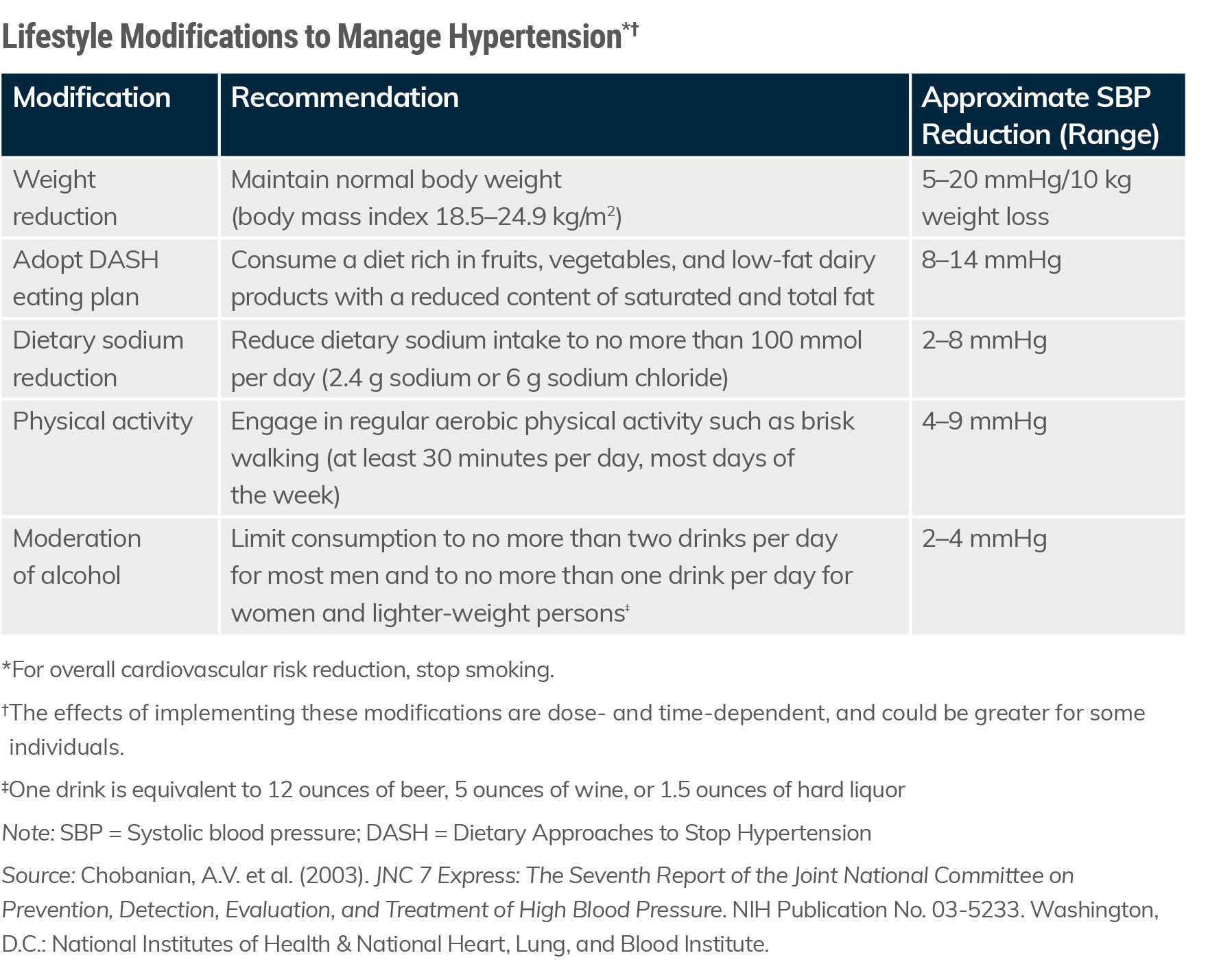
Lifestyle Modifications to Manage Hypertension
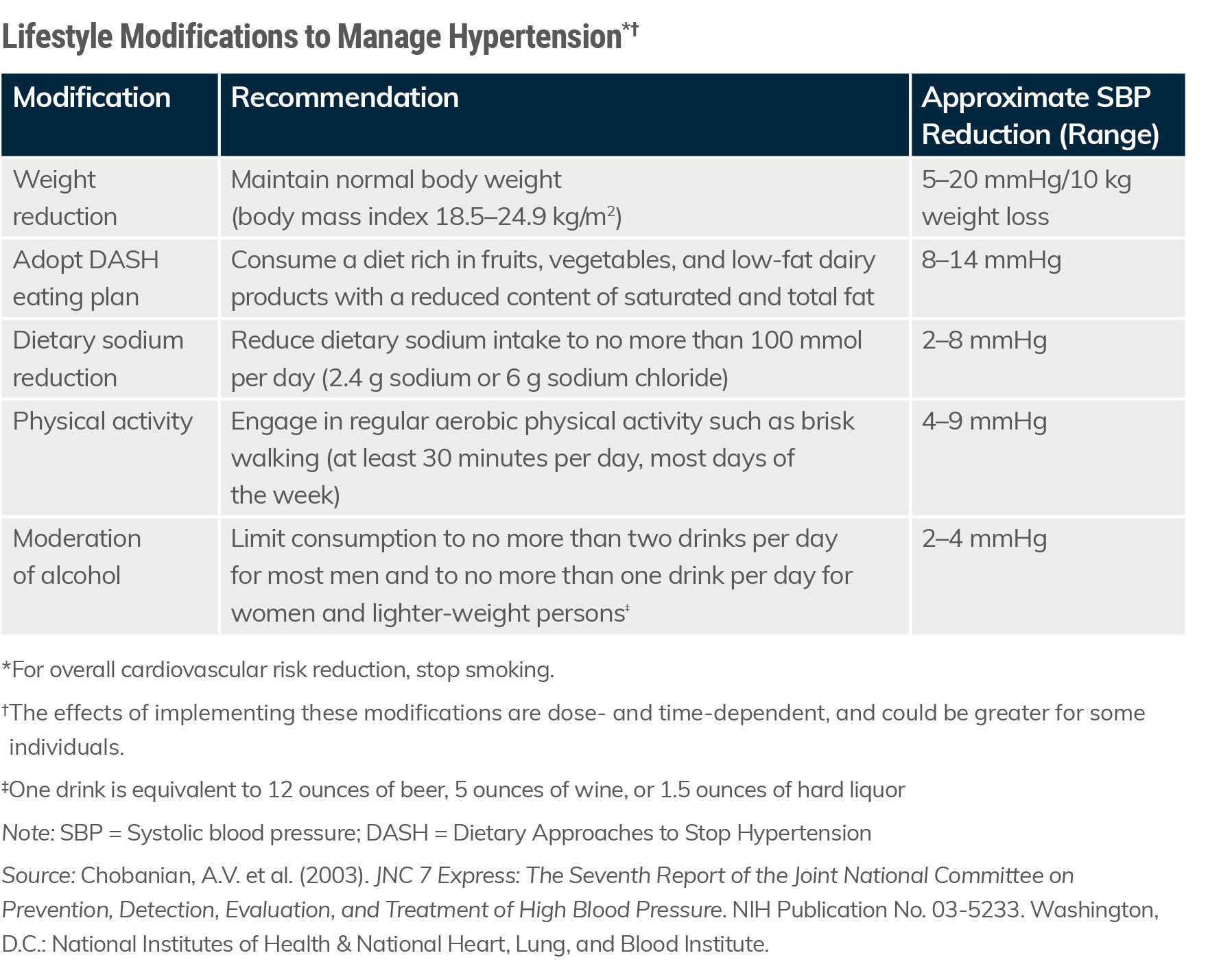
It is widely known that unhealthy lifestyle behaviors contribute to hypertension and there is general agreement that lifestyle modification is important for preventing and managing this condition. Table 3 outlines the lifestyle changes recommended by the American Heart Association to manage hypertension. These include losing weight (especially body fat); reducing alcohol intake; exercising regularly; modifying diet by reducing salt intake and maintaining adequate levels of dietary potassium, magnesium and calcium; and stopping the use of tobacco. Of these, nutrition, exercise and reduced body weight are major factors that can reduce blood pressure. After reviewing the efficacy of diet, nutritional supplements, lifestyle modification and medications for managing hypertension, a group of scientists concluded that there is good evidence that the non-medication antihypertensive strategies can be just as effective as medications and, in some cases, even more effective.
Lifestyle modification can be beneficial for virtually everyone. For example, people with normal blood-pressure levels can benefit from changing unhealthy habits that may increase the risk of developing hypertension. Individuals who have elevated or stage 1 hypertension (see Table 1) are usually advised to modify their lifestyles to see if this will delay or prevent the need to take medication. And, the majority of individuals classified as having elevated blood pressure or stage 1 hypertension can be treated with lifestyle changes instead of medications. If lifestyle modifications fail to reduce blood pressure after three to six months, then medications are usually prescribed. Yet, even in persons with hypertension who are on medication, lifestyle changes that are maintained may reduce the amount of medication needed to control blood pressure. For these reasons, it is worthwhile to work with your clients to help them effectively implement and sustain meaningful and lasting lifestyle changes.
In addition to exercise, nutrition can play a significant role in preventing and managing hypertension. The American Heart Association, American College of Cardiology, and Centers for Disease Control and Prevention all recommend the Dietary Approaches to Stop Hypertension (DASH) eating plan to all persons with hypertension, whether they are attempting to manage the disease with or without medication. The DASH eating plan advocates consuming fiber and potassium via fruits, vegetables and whole grains; reducing sodium intake and total and saturated fat; and getting adequate protein via lean meat and low-fat dairy products instead of high-fat or processed meat. You can play an important role in partnering with clients to explore dietary changes to help them prevent and manage hypertension.
Table 3. Lifestyle Modifications for Managing Hypertension
Use the ACE Mover Method to Help Manage Clients Manage Their Hypertension
To help put this information into context for your work as a health and exercise professional, the following section illustrates how the ACE Mover Method™ and the ACE ABC Approach™ can be used to empower your clients to make behavioral changes that can be incorporated into their lifestyles, align with their values and drive meaningful benefits to their health, fitness and overall quality of life. The underlying philosophy behind the development of these tools is that your job as an exercise professional entails far more than an understanding of sets, repetitions and exercise programming.
An ACE-supported study completed in 2020 examined the effectiveness of the ACE Mover Method at modifying healthy lifestyle behaviors in a group of individuals with varying degrees of blood pressure values ranging from normal to hypertensive. All 28 participants completed a 12-week personalized exercise training program based on the ACE Integrated Fitness Training® (ACE IFT®) Model. In addition to performing the personalized exercise program, half of the participants (the ACE Mover Method group) also received an intervention consisting of weekly client-centered sessions featuring the principles of the ACE Mover Method philosophy and ACE ABC Approach. These sessions were embedded within the normal exercise routine and personalized to each participant’s unique goals and needs. These conversations were collaborations aimed at positive lifestyle changes. Here were the main findings of the study:
- Participants in the ACE Mover Method group experienced statistically significant improvements in all healthy behaviors and lifestyle change categories (i.e., reduced sedentary time, healthy eating and stress reduction) over the course of the 12 weeks.
- The systolic blood pressure reductions in the ACE Mover Method group were 6mmHg. This was 9% greater relative to the group without those interventions.
As mentioned previously, lifestyle interventions are important strategies for managing hypertension. In particular, the ACE Mover Method is one evidence-based strategy that you can use to help your clients make positive lifestyle behavior changes that are likely to coincide with substantial improvements to their blood-pressure profile. Although these changes appear rather minimal, blood-pressure reductions of as little as 2 mmHg are associated with a 6% reduction in stroke mortality and a 4% reduction in coronary artery disease.
Summary
Left untreated, hypertension becomes progressively worse. With adequate treatment, however, blood pressure can be reduced to acceptable levels. By educating yourself about the condition and how certain medications may affect an individual’s exercise response, understanding appropriate exercise programming guidelines and leveraging the ACE Mover Method when warranted, you can set your clients up for success by helping them perform regular exercise and work toward achieving positive lifestyle behavior changes.
Expand Your Knowledge
Looking for more information on how to help clients who deal with chronic health issues? Here are some great resources that also offer opportunities to earn the continuing education credits (CECs) you need to renew your certification.
Mindful Movement: Coaching Clients to Become More Active
Through this Mindful Movement course, you will learn a unique approach to help your inactive clients become physically active. You will be equipped with new coaching techniques and key concepts, plus tools and resources to help them find purpose and enjoyment in movement.
Advanced Behavior Change Strategies for Weight Management
With 67% of Americans reporting they feel more stressed since the pandemic, the need is higher than ever for a “deep health” approach to weight change that centers on the whole person and whole life changes, along with daily actions that support all aspects of health, not just physical health. In this 2-hour video training, you’ll learn a habit-based approach built for individuals impacted by busy and stressful lives. We’ll look at tools built from evidence on the psychology of change, including how to leverage identity, Precision Nutrition’s “goals-skills-practices-actions” framework and how to build a growth mindset in clients.