Breast cancer is one of the most common forms of cancer in women, which means it is likely that you will have clients who are breast cancer survivors. While exercise can provide numerous benefits, it is important to consider certain aspects of the disease when designing exercise programs, including side effects of cancer treatments, exercise barriers, and special concerns for testing and programming. Here are a few considerations for providing safe and effective exercise plans for these clients:
Treatment Side Effects
While survival rates have improved, treatment side effects can negatively impact health, functional ability, and quality of life during and after treatments. In addition, side effects can serve as barriers for exercise participation (Sander et al., 2012). A few side effects to consider are:
- Lymphedema: Patients who undergo surgery or radiation therapy are at risk for developing lymphedema, which results in arm swelling from an accumulation of lymph fluid in the tissue (Sakorafas et al., 2006). This can lead to pain, weakness, and decreased mobility in the shoulder and arm. While there is evidence to support that exercise does not exacerbate lymphedema (Schmitz et al., 2009; Simonavice, Kim and Panton, 2017), it is important to consistently measure arm circumference, monitor lymphedema-related symptoms, and encourage clients to wear compression sleeves. (This CERTIFIED article provides more in-depth information on how to work with clients who have lymphedema.)
- Peripheral Neuropathy: Peripheral neuropathy, which may occur following chemotherapy, can cause hand and foot numbness, muscle weakness and loss of balance (Wickham, 2007). Consider offering additional balance assistance during standing exercises and choose equipment that is easy to grip.
- Body Composition and Bone Mineral Density: Breast cancer treatments can cause accelerated gains in fat mass and losses in muscle and bone mineral density (BMD). These changes lead to strength and functional limitations, increased risk for bone fractures and osteoporosis. Special emphasis should be placed on programming that positively affects body composition and BMD.
- Fatigue: Cancer-related fatigue is experienced by a majority of women undergoing chemotherapy or radiation therapy (Stasi et al., 2003). It can last long after treatment and can negatively impact breast cancer survivors’ ability to perform activities such as walking, exercising, lifting objects and climbing stairs (Curt et al., 2000). Be sure to monitor your clients’ fatigue levels during training sessions and take these observations into consideration when determining the intensity and volume of your clients’ programs.
Exercise Programming
Before beginning an exercise program, talk with your client to determine if any treatment-related side effects are present. Then, decide on the appropriate fitness tests to administer based on present side effects as well as your client’s overall health. Once you have established baseline fitness values, use the results to determine an appropriate fitness program. A comprehensive program should include:
- Stretching: Stretching exercises are essential to help your client regain range of motion in the affected arm (the side where cancer was present). Encouraging your client to participate in a gentle or restorative yoga class may be beneficial, as yoga has been found to increase arm range of motion, reduce arm pain and swelling, and improve fatigue and quality of life in breast cancer survivors (Andysz et al., 2014; Bower et al., 2012).
- Cardiovascular Training: Cancer treatments can negatively affect the cardiovascular system. Therefore, aerobic training is a necessary program component for increasing cardiovascular fitness. In addition, more research is supporting the use of high-intensity interval training (HIIT) as a safe and effective intervention for breast cancer survivors (Devin et al., 2016; Schmitt et al., 2016). Aerobic exercise programming for breast cancer survivors should follow the same physical-activity guidelines given for healthy populations, keeping in mind any treatment-related side effects (Schmitz et al., 2010).
- Strength Training: Strength training can help combat the treatment-related losses in muscle mass, BMD, strength and physical function. While HIIT (60-80% of 1RM) has been shown to be well tolerated by breast cancer survivors (Madzima et al., 2017), it is recommended to start with low resistance and slowly progress in small increments while monitoring lymphedema symptoms and pain (Schmitz et al., 2010).
- High-impact Training: Incorporating high-impact movements in combination with strength training may produce additional benefits for BMD compared to resistance training alone (Zhao, Zhao and Xu, 2015; Winters-Stone et al., 2013). Before adding impact exercises, make sure clients can perform low-impact exercises with proper form and are at an appropriate fitness level to perform higher-impact movements. Then, gradually add in movements such as hops, jumps or squat jumps.
Final Tips
Once you create an exercise program for your client, be sure to keep in mind the following:
- Warm-up: Provide a warm-up to gradually increase joint range of motion and to assess how your client is feeling early on in the workout.
- Gradually Progress: Start with lower intensity, duration and frequency, and gradually progress while monitoring cancer-related side effects.
- Monitor Clients: Monitor client’s fatigue, pain levels and symptoms throughout the session and adjust intensity accordingly.
References
Andysz, A. et al. (2014). Effect of a 10-week yoga programme on the quality of life of women after breast cancer surgery. Przegla?d Menopauzalny, 13, 3, 186-93.
Bower, J.E., et al. (2012). Yoga for persistent fatigue in breast cancer survivors: A randomized controlled trial. Cancer, 118, 15, 3766-3775.
Devin, J.L. et al. (2016). The influence of high-intensity compared with moderate-intensity exercise training on cardiorespiratory fitness and body composition in colorectal cancer survivors: A randomised controlled trial. Journal of Cancer Survivorship, 10, 3, 467-479.
Madzima, T.A. et al. (2017). Effects of resistance training and protein supplementation in breast cancer survivors. Medicine and Science in Sports and Exercise, 49, 7, 1283-1292.
Sakorafas, G.H. et al. (2006). Lymphedema following axillary lymph node dissection for breast cancer. Surgical Oncology, 15, 3, 153-165.
Sander, A.P. et al. (2012). Factors that affect decisions about physical activity and exercise in survivors of breast cancer: A qualitative study. Physical Therapy, 92, 4, 525-536.
Schmitt, J. et al. (2016). A 3-week multimodaA intervention involving high-intensity interval training in female cancer survivors: a randomized controlled trial. Physiological Reports, 4, 3.
Schmitz, K.H. et al. (2009). Weight lifting in women with breast-cancer-related lymphedema. The New England Journal of Medicine, 361, 7, 664-673.
Schmitz, K.H. et al. (2010). American College of Sports Medicine Roundtable on exercise guidelines for cancer survivors. Medicine & Science in Sports & Exercise, 42, 7, 1409-1426.
Simonavice, E., Kim, J.-S. and Panton, L. (2017). Effects of resistance exercise in women with or at risk for breast cancer-related lymphedema. Supportive Care in Cancer, 25, 1, 9-15.
Stasi, R., et al. (2003). Cancer-related fatigue: Evolving concepts in evaluation and treatment. Cancer, 98, 9, 1786-1801.
Wickham, R. (2007). Chemotherapy-induced peripheral neuropathy: A review and implications for oncology nursing practice. Clinical Journal of Oncology Nursing, 11, 3, 361.
Winters-Stone, K.M. et al. (2013). Impact + resistance training improves bone health and body composition in prematurely menopausal breast cancer survivors: A randomized controlled trial. Osteoporosis International, 24, 5), 1637-1646.
Zhao, R., Zhao, M., and Xu, Z. (2015). The effects of differing resistance training modes on the preservation of bone mineral density in postmenopausal women: A meta-analysis. Osteoporosis International, 26, 5, 1605-1618.




 by
by 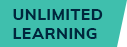






 by
by