In the past two decades, diabetes rates in the United States have increased significantly. According to the Centers for Disease Control and Prevention, nearly 30 million Americans have diabetes—that’s 10% of the population. Another 86 million Americans are thought to be living with prediabetes—a condition in which blood glucose levels are above normal, but not high enough to be classified as diabetes. Public health experts estimate that one in three Americans will have diabetes by 2050 (Centers for Disease Control and Prevention, 2014). Individuals with diabetes who are able to manage their condition can lead a full life, but uncontrolled diabetes can lead to amputations, vision loss, heart and kidney diseases, and even premature death.
What is Diabetes?
Diabetes mellitus is a group of diseases characterized by persistently high levels of blood glucose. In a healthy person, carbohydrates are broken down into glucose, which the body’s cells use for energy. When glucose enters the bloodstream, insulin (a hormone secreted by the pancreas) signals the body’s cells to take up glucose from the bloodstream and transport it into the cell where it can be used for immediate energy. Insulin also mediates the process of converting glucose that is not needed immediately to glycogen so that it can be stored in the liver and muscles for later use. When glucose levels drop, the pancreas stops secreting insulin until more glucose enters the bloodstream.
Type 1 diabetes (T1D)—or insulin-dependent diabetes—is an autoimmune disease in which a person’s immune system destroys the insulin-producing beta cells of the pancreas. T1D is the more serious form of diabetes and accounts for approximately 5% of diabetes cases. It is thought that a genetic variant predisposes certain people to T1D. People with T1D must take insulin injections or infusions daily.
Type 2 diabetes (T2D)—or non-insulin dependent diabetes—accounts for the majority (90-95%) of diabetes cases. In T2D, the body produces insulin, but isn’t able to use it properly. Both genetics and lifestyle play a role in the development of T2D (American Diabetes Association, 2018). Type 2 diabetes typically develops slowly. In the early stages, cells throughout the body become resistant to the effects of insulin—a condition known as insulin resistance. Over time, the body may stop producing sufficient insulin altogether. The processes of glucose uptake by the body’s cells and the conversion of glucose to glycogen begin to fail. The consequence is higher levels of circulating blood glucose.
How to Reduce Your Risk of Diabetes: 5 Things You Can Do
Risk Factors
Diabetes is caused by a combination of environmental factors, lifestyle behaviors and genetic susceptibility. Nonmodifiable risk factors include age, ethnicity, family history and biological factors. While these factors play a critical role in a person’s risk for developing diabetes, several risk factors can be controlled. Read on to learn how to reduce your risk for diabetes.
- Eat more whole grains.
A healthful diet in general is associated with a decreased risk of diabetes. However, one dietary habit in particular seems to have a profound effect on a person’s risk for diabetes: consumption of whole grains. There is strong evidence that diets abundant in whole grains have a protective effect against the development of diabetes (van Dam et al., 2002). The bran and fiber found in whole grains such as quinoa, brown rice and whole-grain breads help to stabilize blood glucose levels in the body. Refined grains, such as white bread, donuts and sugary cereals, have the opposite effect and produce spikes in blood glucose levels. The Dietary Guidelines for Americans recommend making half the grains you eat whole. Additionally, a prospective cohort study published by the Public Library of Sciences found that women who averaged two to three servings of whole grains a day were 30% less likely to develop type 2 diabetes than those who seldom consumed whole grains (de Munter et al., 2007). - Get enough sleep.
You know that sleep is important for feeling your best every day, but did you know that chronic sleep deprivation could influence your risk of diabetes? People who are sleep deprived are at an increased risk for metabolic syndrome, which is a combination of risk factors that often precipitates chronic disease, including diabetes. One symptom of metabolic syndrome is impaired glucose metabolism—a sign of prediabetes. Chronic sleep deprivation can alter your body’s hormone regulation, causing less insulin to be produced and an increase in stress hormones such as cortisol. The aggregate effect is potentially elevated glucose in the bloodstream (National Sleep Foundation, 2018). Aim for at least seven hours of quality sleep each night. If you have trouble falling asleep or staying asleep, evaluate your personal sleep habits. Sleep can often be improved by adopting a few simple sleep hygiene promoting behaviors. If you think your sleep problems are more serious, talk to your doctor. - Get at least 150 minutes of aerobic exercise each week.
You’ve heard for years that exercise can improve your overall health. According to the American Diabetes Association, two types of exercise are important for reducing your risk for diabetes: aerobic exercise and strength training (American Diabetes Association, 2018). Aerobic exercise helps your body use insulin more efficiently. Thirty minutes of moderate-intensity exercise at least five days a week is the goal, but if 30 minutes seems overwhelming in the beginning, start with 10-15 minutes and build from there. -
Do strength training.
The other type of exercise that can help to reduce your risk of developing diabetes is strength training. While aerobic exercise helps your body use insulin more efficiently, strength training makes your muscle cells more sensitive to insulin, which helps to lower blood glucose levels. Use the following industry guidelines to plan your strength-training program:- Select eight to 10 exercises that target the major muscle groups.
- Choose multijoint exercises (those affecting more than one muscle group) over single-joint exercises.
- Train each muscle group for a total of two to four sets, completing eight to 12 repetitions per exercise.
- Perform resistance-training exercises for each major muscle group two to three nonconsecutive days per week, with at least 48 hours of recovery between sessions.
- Manage your stress.
Try to do something stress-reducing daily. According to the American Diabetes Association, stress management plays an important role in reducing the risk of type 2 diabetes and managing the disease after a diagnosis. Lifestyle behaviors associated with unchecked stress, such as poor sleep hygiene, poor eating habits and lack of adequate physical activity, increase a person’s risk for diabetes, but stress hormones such as cortisol may have a direct effect on blood glucose levels (Virtanen et al., 2014). The stress paradox can make it seem impossible to fit in stress-reducing activities such as exercise or meditation when you already feel like you’re spread too thin. But even just a few minutes of deep breathing every day can help to subdue your body’s fight or flight stress response.
To learn more about diabetes and what you can do to reduce your risk, visit www.diabetes.org.
References
American Diabetes Association (2018). Diabetes Basics.
American Diabetes Association (2018). Diabetes Food and Fitness.
Centers for Disease Control and Prevention (2014). National Diabetes Statistics Report.
de Munter, J.S. et al. (2007). Whole grain, bran, and germ intake and risk of type 2 diabetes: A prospective cohort study and systematic review. Public Library of Sciences Journal of Medicine, 4, 8, 1385-1395.
National Sleep Foundation (2018). The link between lack of sleep and type 2 diabetes.
van Dam, R.M. et al. (2002). Dietary patterns and risk for type 2 diabetes mellitus in U.S. men. Annals of Internal Medicine, 136, 201-209.
Virtanen, M. et al. (2014). Psychological distress and incidence of type 2 diabetes in high-risk and low-risk populations: The Whitehall II Cohort study. Diabetes Care, 37, 8, 2091–2097.




 by
by 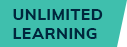





 by
by