Sleep disruption is a growing concern in America. One in three American adults don’t get the recommended seven to nine hours of sleep per night, to the detriment of their overall health (Watson et al., 2015). A consensus statement published in the Journal of Sleep Medicine suggests that despite needing 10-12 hours of sleep per night, many kids ages five to 10 years old are falling short (Paruthi et al., 2016). It appears that, like adults, less than optimal sleep increases children’s risk for a variety of health problems.
Of these sleep-related health problems, childhood obesity is an increasing focus of concern.
Sleep is a “planned” time for recovery in our human biorhythms that allows for tissue growth and repair. High rates of hormonal activity during sleep help regulate a variety of physiological processes that impact growth, cognition and behavior. When sleep is compromised, so are all of the above. Given how rapidly children’s brains and bodies are growing, a lack of sleep can be disruptive to the developmental process.
Research on how this disruption may contribute to increased rates of obesity has presented some significant findings:
- Data published in the Archives of Pediatric and Adolescent Medicine suggests in young children (0-4 years), shortened nighttime sleep was associated with increased risk of having overweight and/or obesity. Daytime sleep (naps) did not improve risk (Bell and Zimmerman, 2010).
- A study published in Pediatrics revealed that kids ages four to 10 years with the shortest sleep durations were four times more likely to have obesity. Short and inconsistent sleep duration was also associated with altered insulin, low-density lipoprotein (LDL) cholesterol levels and C-reactive protein (Spruyt et al., 2010).
- Research from the University of Illinois, Urbana-Champaign examined family routines and subsequent health outcomes. Their findings suggest that kids sleeping fewer than seven hours per night are three times more likely to become overweight. Additionally, kids of parents getting fewer than seven hours of sleep per night were 1.3 times more likely to become overweight. The researchers concluded that sleep may be one of the most important early factors to target in childhood obesity prevention (Jones et al, 2014).
These findings are not limited to the acute impact of sleep on childhood obesity. It appears that the risk of developing obesity from insufficient sleep during childhood may extend into adulthood.
- A study of more than 1,000 people in New Zealand discovered shorter sleep times in childhood increased the likelihood of having obesity by age 32 (Landhuis et al., 2008).
- A systematic review of more than 36 publications published in Obesity found a significant link between short sleep duration during childhood and lifelong obesity (Patel and Hu, 2017).
How Are Childhood Obesity and Lack of Sleep Related?
Researchers report that while there are some important findings, it is difficult to determine exactly why and how sleep impairment impacts childhood obesity. Some suggest it could be somewhat of a “chicken or the egg” phenomenon. Rates of sleep disturbances such as sleep apnea are much higher in children who have obesity. However, the commonly proposed mechanisms by which sleep impacts obesity are similar in adults and children.
Hunger Hormone Imbalance
When sleep is impaired at any age, the hormone leptin decreases significantly. This hormone signals the brain that it’s time to stop eating. This decrease is paired with an increase in the hormone ghrelin, which increases one’s affinity for food, resulting in a higher caloric intake (Teheri et al., 2004).
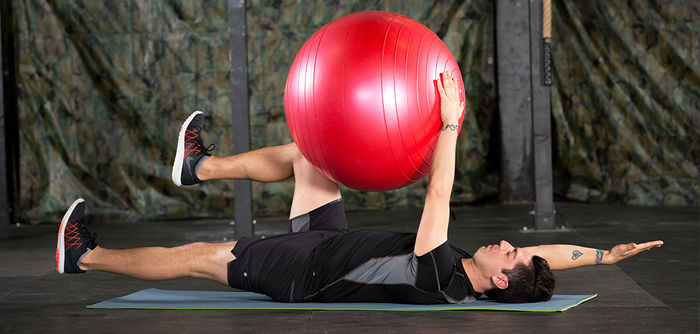
Decreased Energy Expenditure
Insufficient sleep lowers core temperature, which contributes to fatigue. Fatigued adults and children are less likely to be physically active (Stone et al., 2012).
Increased Cortisol Levels
It’s been observed that suboptimal sleep can acutely increase the stress hormone cortisol. Chronic increases in cortisol have been linked to insulin resistance and increased bodyweight in both adults and children (Speigel et al., 2015).
These findings make it clear that sleep plays a role in the childhood obesity epidemic. There are, however, pro-active steps parents can take to help improve their children’s sleep patterns.
Limit technology prior to bedtime. Watching television immediately prior to bedtime has been associated with impaired sleep duration in children (Owens et al., 1999). Turning off the television and other screen devices at least 30 minutes prior to bedtime is often recommended by physicians and researchers.
Maintain consistent bedtimes. Children’s physiology and psychology respond well to routine. Going to bed and waking up at the same time each day aids in creating an optimal sleep/wake cycle (Blader et al., 1997). With increasing external time constraints (school and other activities), it’s essential that parents and educators evaluate the purpose of these demands for time. While children need to learn how to apply rigor to various disciplines, it’s also essential they are provided time for physical play and relaxation.
Use common sense. Remember that quality sleep is optimal when children go to bed in a calm state. Any highly stimulating activities prior to bedtime are contrary to this goal. Consider different measures and rituals that can be performed prior to bedtime that promote calmness and relaxation.
Even with our best efforts as parents, we’ll still be getting glasses of water and checking under the bed for monsters at 2 a.m. However, realizing the important relationship between children’s sleep and their health, we can take steps to make nighttime rest a time to recharge happy, healthy young lives.
List of References
Bell, J.F. and Zimmerman, F.J. (2010). Shortened nighttime sleep duration in early life and subsequent childhood obesity. Archives of Pediatrics & Adolescent Medicine, 164, 9.
Blader, J.C. (1997). Sleep problems of elementary school children: A community survey. Archives of Pediatrics and Adolescent Medicine, 151, 5, 473.
Jones, B.L. and Fiese, B.H. (2014). Parent routines, child routines and family demographics associated with obesity in parents and preschool-aged children. Frontiers in Psychology, 5.
Landhuis, C.E. et al. (2008). Childhood sleep time and long-term risk for obesity: A 32-year prospective birth cohort study. Pediatrics, 122, 5, 955–960.
Owens, J. et al. (1999). Television-viewing habits and sleep disturbance in school children. Pediatrics, 104, 3.
Paruthi, S. et al. (2016). Recommended amount of sleep for pediatric populations: A consensus statement of the American Academy of Sleep Medicine. Journal of Clinical Sleep Medicine, 12, 06, 785–786.
Patel, S.R. and Hu, F.B. (2008). Short sleep duration and weight gain: A systematic review. Obesity, 16, 3, 643–653.
Spiegel, K. et al. (2004). Leptin levels are dependent on sleep duration: Relationships with sympathovagal balance, carbohydrate regulation, cortisol and thyrotropin. The Journal of Clinical Endocrinology & Metabolism, 89, 11, 5762–5771.
Spruyt, K., Molfese, D.L. and Gozal, D. (2011). Sleep duration, sleep regularity, body weight, and metabolic homeostasis in school-aged children. Pediatrics, 127, 2.
Stone, M.R., Stevens, D. and Faulkner, G.E. (2013). Maintaining recommended sleep throughout the week is associated with increased physical activity in children. Preventive Medicine, 56, 2, 112–117.
Taheri, S. et al. (2004). Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Medicine, 1, 3.
Watson, N.F. et al. (2015). Recommended amount of sleep for a healthy adult: A joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Journal of Clinical Sleep Medicine, 11, 06, 591–592.




 by
by