As national obesity rates have continued to rise, so too have various, often opposing, theories on the health implications of excess weight. One such theory is called Health at Every Size (HAES), a weight-neutral approach built on the following principles:
- Acceptance of natural body diversity in weight and size
- Ineffectiveness and danger in dieting for weight loss
- Eating in response to internal body cues
- Recognition of social, emotional and spiritual factors in addition to physical factors related to health and happiness (Robison, 2005)
The HAES movement is largely credited to Linda Bacon, Ph.D., who introduced the concept in her book Health at Every Size: The Surprising Truth About Your Weight, which refutes the idea that overweight and obesity cause adverse health outcomes (Bacon, 2010). Bacon presents data supporting the idea that behaviors, not weight, are most important in the development of poor health.
This article explores the research supporting and refuting HAES and offers strategies to encourage healthy behavior change among clients who struggle with excess weight.
Support for Health at Every Size
A large body of evidence suggests a correlational link between obesity and numerous chronic health conditions such as diabetes, hypertension and arthritis (Kearns et al., 2014). Despite this correlational link, there is little direct evidence showing that obesity causes these conditions (Bombak, 2014). The current treatment of obesity-related conditions involves encouraging weight loss via dietary restriction and increased exercise in an attempt to improve health outcomes.
However, these common weight-loss strategies have little supporting evidence for long-term weight loss. In fact, dieting has been shown to lead to weight gain in roughly two-thirds of dieters within the one to five years following their diet (Mann et al., 2005). Often, failed dieting attempts increase feelings of self-blame and an attitude of "If nothing works I may as well just go back to what I was doing before." Despite the tendency for self-blame, numerous mechanisms, such as increased hunger, reduced satiety and reduced energy expenditure, may be partially to blame for increased weight gain post-dieting (Bombak, 2014).
Beyond dieting's poor effectiveness, it's also been shown to increase rates of both eating disorders and obesity (Haines and Neumark-Sztainer, 2006).
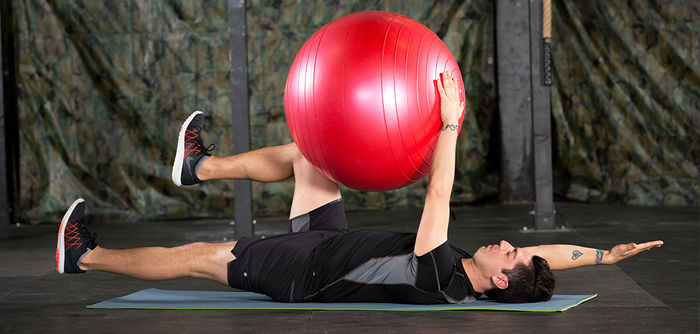
Finally, evidence suggests that healthy behaviors, such as regular exercise and nutritious eating, positively impact health regardless of a change in weight (Bacon and Aphramor, 2011; Duncan et al., 2003). Additionally, research has shown that individuals who are overweight but active have lower mortality rates than their normal-weight but non-exercising peers (Blair and Church, 2004).
In light of this evidence, HAES suggests that exercise and medical professionals shift their attention away from weight and focus instead on the adoption of sustainable healthy behaviors. These behaviors include consumption of healthful foods, following internal hunger and satiety cues, engaging in enjoyable exercise and avoiding fat stigma.
Randomized control trials using a HAES model have shown improved outcomes in blood biomarkers, eating behaviors and psychological outcomes, including mood, self-esteem and body image (Bacon and Aphramor, 2011).
Arguments Against Health at Every Size
HAES critics have two main opposing arguments. First, they argue that there is ample evidence that shows excess adiposity is related to chronic disease, especially in those who fall under class II (moderate-risk) or class III (high-risk) obesity. Second, that the concept of listening to internal hunger and satiety cues is challenging in our obesogenic environment. They further argue that the HAES studies showing positive outcomes have utilized small sample sizes with individuals who are overweight or with class 1 obesity, excluding those with class II or III obesity, for whom weight loss may be more beneficial (Penney and Kirk, 2015).
While they acknowledge that the HAES approach may be useful, they insist on more evidence with larger and more diverse sample sizes to assess if the approach is truly beneficial for both individual and population-level health.
Where to Go From Here
Whether or not HAES resonates with you, your clients can benefit from a training approach that focuses on more than just weight. It may never have occurred to your client that there are benefits of exercise and healthy eating besides weight loss.
Armed with this information, there are two powerful ways you can encourage healthy behavior change. First, educate your clients. Let them know that their behaviors matter in regards to their health and quality of life, whether or not those behaviors lead to weight loss. Second, help them build an expanded view of the benefits of exercise. Rather than only setting a weight-loss goal, encourage clients to track changes related to blood biomarkers, reduced stress or anxiety, better sleep and energy, or improvements in sport and activities of daily living.
Once clients realize the powerful life-enhancing benefits of exercise, they’re more likely to make it a sustainable habit, regardless of weight outcomes.
Learn more about healthy behaviors with a behavior change specialist program.
Works Cited
- Bacon, L. (2010). Health at Every Size: The Surprising Truth about your Weight. Dallas, Texas: BenBella Books.
- Bacon, L. and Aphramor, L. (2011). Weight science: Evaluating the evidence for a paradigm shift. Nutrition Journal, 10, 9.
- Bombak, A. (2014). Obesity, Health at Every Size, and public health policy. American Journal of Public Health, 104, 2, e60–e67.
- Duncan, G.E. et al. (2003). Exercise training, without weight loss, increases insulin sensitivity and postheparin plasma lipase activity in previously sedentary adults. Diabetes Care, 26, 3, 557–562.
- Haines, J. and Neumark-Sztainer, D. (2006). Prevention of obesity and eating disorders: A consideration of shared risk factors. Health Education Research, 21, 6, 770–782.
- Kearns, K. et al. (2014). Chronic disease burden associated with overweight and obesity in Ireland: The effects of a small BMI reduction at population level. BMC Public Health, 14, 143.
- Penney, T.L. and Kirk, S.F.L. (2015). The Health at Every Size paradigm and obesity: Missing empirical evidence may help push the reframing obesity debate forward. American Journal of Public Health, 105, 5, e38–e42.
- Robison, J. (2005). Health at Every Size: Toward a new paradigm of weight and health. Medscape General Medicine, 7, 3, 13.




 by
by