One of the most common chronic conditions among people over the age of 50 is osteoarthritis, which is a progressive degenerative condition that worsens over time due to destructive thinning of the cartilage. This leads to pain and dysfunction, including strength, range-of-motion and functional deficits. Common treatments include exercise, nonsteroidal anti-inflammatory medications and heat/ice. However, once all of the cartilage is lost, these treatments are ineffective and more intensive options need to be explored. Total joint replacement has become a routine treatment, and the two most common joints to undergo the procedure are the hips and knees. According to the American Academy of Orthopaedic Surgeons, osteoarthritis is the leading cause of knee replacement and 90% of patients report a significant improvement in symptoms following the procedure.
In 2010, approximately 2.5 million people were living with total hip arthroplasties (THA) and 4.7 million people with total knee replacements (TKR) in the U.S. (Kremers, 2015). Currently, more than 700,000 total knee replacement surgeries take place annually and that number is expected to increase significantly to 3.5 million annually by the year 2030. Given the continued increase in the number of people undergoing joint replacement surgery, as a health and exercise professional it is essential that you have the knowledge and skills to be able to work with these clients, both before and after their procedures. This article summarizes the rehabilitative process and exercise recommendations for these clients.
The Rehabilitative Process
Acute post-operative physical therapy often starts the day after surgery to start working on improving range of motion, basic strengthening, gait training and stair climbing. The typical hospital stay is only about four days unless there are complications. Once released from the hospital, a patient may receive some home therapy before being referred to an outpatient clinic. During outpatient therapy, the main focus is to maximize strength, range of motion and functional mobility (including gait and balance). Although exercises after TKR will be more “knee dominant” and exercises after THA will be more “hip dominant,” each of these programs will include knee and hip exercises as they are both important in the kinetic chain to restore functional movement.
Immediately after THA and early in the rehabilitative process (60-90 days typically), the patient will likely be instructed to avoid hip flexion past 90 degrees, crossing the operated leg over the other, and walking pigeon-toed (internal hip rotation). Recovery time is similar for both procedures and it typically takes about two to three months post-surgery to return to a “normal” level of functioning. During therapy, the patient will be asked to perform a home exercise program to maximize his or her recovery progress and it is important that the program is adhered to for best results.
Exercises for THA and TKR
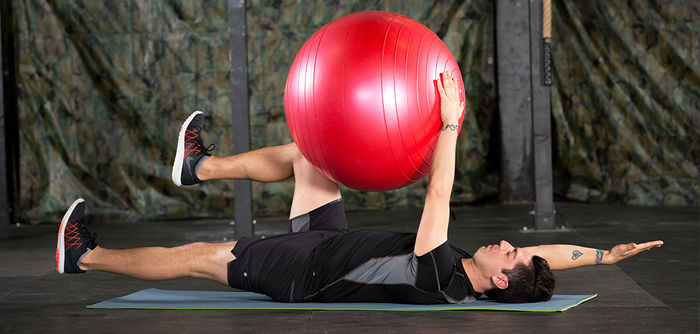
When working with a client who is still undergoing the rehabilitative process or who has just been released, it is important to directly communicate with his or her physical therapist to obtain input regarding what types of exercises to include or avoid in the client’s program. Ask your clients if they have been given a home exercise routine by their physical therapist upon discharge, as this can also be useful information in developing their new program. Exercise at this stage may include a mix of exercises to target the individual muscle groups (e.g., hamstrings, glutes, quads, calves) and more functional or whole-body patterns such as squats, deadlifts and lunges. Balance work may also be a continued component.
In most cases, clients who have undergone joint replacement surgery will have few long-term exercise limitations and their function should improve dramatically because they will no longer be experiencing the pain and discomfort of an osteoarthritic joint. However, if an individual has lived with a painful hip or knee for many years, he or she will have likely developed dysfunctional movement compensations that will need to be addressed. Therefore, these clients should be screened to identify their deficits. Other assessments for strength, gait and balance may also be incorporated, depending on the client’s age and ability level.
Ultimately, it is important to progress these clients to loaded movement patterns. Unilateral lower-body exercises such as step-ups, single-leg stands and forward lunges can reveal deficits in one limb compared to the other, while three-dimensional movements such as clock/matrix lunges, ViPR flow routines and even farmer’s walks can facilitate “linkages” in the kinetic chain. Dynamic balance and agility training, such as agility ladders or obstacle courses, may be incorporated to continue to challenge proprioception and coordination.
Potential Problems
If full motion (0-110 degrees) has not been achieved after TKR, range-of-motion exercises should also be included. It may also be necessary to refer the client back to physical therapy for additional considerations, such as aggressive physical therapy, manipulation under anesthesia, surgical removal of scar tissue or even revision knee replacement (only about 1-2% need a revision). Some patients may report noises such as clicking or popping when bending the knee. This is typically not a concern unless there is pain associated with the noise.
Summary
As a health and exercise professional, don’t be scared off by potential clients who have undergone total joint replacement surgeries; instead, take the time to acquire the skills and knowledge necessary to address the challenges these clients may face. By understanding the rehabilitative process and communicating with therapists, you can help these clients achieve an even higher level of health, function and fitness through proper exercise programming and supervision.




 by
by 









 by
by