In honor of Breast Cancer Awareness Month, and my mother who is fighting her third breast cancer battle, I wanted to share this important information for health and exercise professionals working with breast cancer survivors.
The most common issues that plague post-mastectomy patients are upper-crossed syndrome and range-of-motion limitations in the affected shoulder. Upper cross syndrome is the combination of protracted (rounded) shoulders, forward head, cervical lordosis, winged-scapula and thoracic kyphosis. As a result of these postural deviations, mastectomy, lymph node dissection and/or radiation, the chest muscles may become tight, shortened and spastic. This not only exacerbates the postural deviations, it may also limit the ability of the patient to move their arm/shoulder through flexion, extension, abduction and external rotation. While this is a general statement, the majority of patients will present with these symptoms. This is compounded even more if the woman undergoes reconstructive surgery. In addition to further exacerbating upper-crossed syndrome, it may create a muscle imbalance in the area of surgery, if either the rectus abdominis or latissimus muscle are used for reconstruction.
Program Safety
The most important factor in the safety and efficacy of the exercise program is the initial assessment, which, at the very least, should include a comprehensive postural assessment as well as shoulder range-of-motion measurements taken with a goniometer. The well-trained exercise professional will be able to deduce, from the results, which muscles need to be stretched and which need to be strengthened. By selecting the wrong combinations of exercises, the results may not only be undesirable, they may actually be detrimental. For example, if a client presents with moderate to severe upper-crossed syndrome, performing any kind of “pushing” exercise that involves the chest muscles (chest press) could make the syndrome even more pronounced by causing the pectoral muscles to tighten and contract. Instead, the focus should be on stretching the chest wall and strengthening the opposing muscles in the back, particularly the scapular stabilizers.
Prior to adding a load (resistance) of any kind, the client should have close to full range of motion through the particular plane of motion. Without correcting the range of motion first, the client will reinforce the negative movement pattern by performing strength-training exercises throughout a limited pattern of movement. Therefore, the focus should initially be on range-of-motion exercises. This may include very basic exercises that the client can do on their own, such as front wall walks, side wall walks, pendulum swings and corner stretches; active isolated stretching may also be used with assistance. In most cases, using a combination of movements will increase the speed of improvement.
Strength Training
Once close to full range of motion is achieved, the focus can shift to strength training. Not only will this help to correct the postural and range-of-motion deviations, it will help increase bone density and lean muscle mass as well. Many women will either be of menopausal age or thrown into menopause from their cancer treatment. With estrogen no longer being produced, the risk of osteoporosis increases. To make things even more complicated, the long-term side-effects of chemotherapy include osteoporosis, diabetes and damage to the heart and lungs, all of which can be avoided or improved through proper exercise recommendations.
Mitigating the Risk of Lymphedema
The last part of the equation is the risk of lymphedema of the affected arm/shoulder. Lymphedema is the swelling of the extremity following the removal of, or radiation to, the lymph nodes on that side. Even if someone has undergone a sentinel node biopsy and had just one node removed, they can still get lymphedema. Lymphedema is progressive if untreated and can be very painful and disfiguring. It can happen at any time after surgery—within one hour or 50 years. While the risk doesn’t increase or decrease with time, a higher percentage of body fat, infection, age and poor nutrition can all increase the risk once someone is at risk. In my 16 years of working with cancer patients, I believe this to be the number one “overlooked” issue among cancer patients. More often than not, they will not even be told about lymphedema. Following lymph node dissection and/or radiation, the lymphatic pathways do not operate with the same efficacy that they did prior to treatment. Therefore, we no longer know the individual’s exercise threshold. It is critical to start and progress slowly, which allows for a gradual increase in frequency, intensity and duration of the exercise program. If at any point there is swelling, the client should be advised to stop exercising and see their doctor immediately to determine if, in fact, they do have the onset of lymphedema. They should come back with a medical clearance form and the exercise professional should reduce the frequency, intensity and duration to the point prior to the onset of swelling.
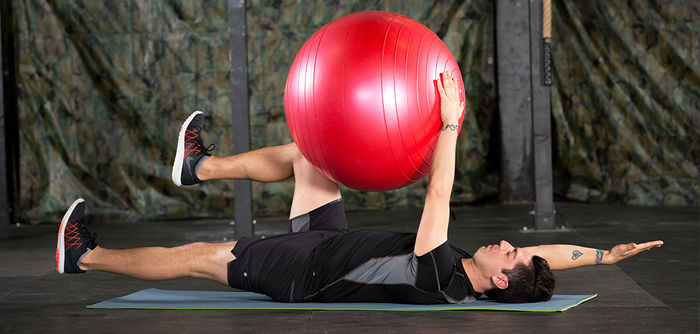
Putting all of these pieces together is very much like solving a mathematical equation. If you are missing any of the information, you will never solve the problem. A typical exercise session should begin with cardiovascular exercise. This should be gradually increased at a rate that is comfortable to the client. They should stay well-hydrated, avoid wearing tight-fitting or restrictive clothing on their upper body, and be cautious not to overheat (all of these factors can increase the risk of lymphedema). Following the warm-up, have the client perform a series of lymph-drainage exercises to open up the lymphatic pathways and prepare the body for exercise. I reference these exercises in CETI’s Cancer Exercise Specialist Handbook and Breast Cancer Recovery with the BOSU® Balance Trainer Book.
Following the warm-up and lymph-drainage exercises, determine what the areas of “need” are for the client. Remember to begin with stretching and range of motion exercises until they have close to “normal” range of motion. At that point, the focus shifts to strength training and choosing exercises that will strengthen the weaker muscles and stretch the tight and shortened muscles. Increase resistance gradually and attention paid to any potential swelling of the extremity. Typically, I chose exercises that stretch the chest (chest fly, corner or door stretch, assisted stretching) and strengthen the back (low/high rows, reverse flies, lat pulldown). Clients often present with winged scapula following a node dissection. If this is the case, I incorporate exercises that strengthen the serratus anterior. If they have undergone an abdominal TRAM procedure, core work will be of the greatest importance in preventing or minimizing low-back pain.
Because every muscle in the body works synergistically, an imbalance in the shoulder can lead to a multitude of imbalances from the hips to the knees to the ankles. Choose your exercises carefully and emphasize the areas of need. No two breast cancer patients are the same. Not only are you taking into consideration their surgery, reconstruction and treatment, you have to also factor in the remainder of their health history and any additional orthopedic concerns. I urge anyone who wants to work with cancer patients to undergo specialized training. It is very complex, and the untrained professional can end up doing more harm than good.




 by
by