|
Key Takeaways To support your immune system, live a healthy lifestyle, which can be defined using the 6 pillars of lifestyle medicine: nutrition, physical activity, stress management, avoidance of risky substances, restorative sleep and positive social connections. The associations between a healthy lifestyle and immune system function are clearly established and supported by science, so read on to learn how making small changes related to each of those pillars can optimize your immune system and lead to a longer and healthier life. |
The first line of support for maintaining a vigorous immune system is leading a healthy lifestyle, which includes a healthy diet, physical activity, stress management, avoidance of smoking and the use of other risky substances, restorative sleep and positive social connections. Read on to learn more about how leading a healthy lifestyle can support an optimally functioning immune system.
What is the Immune System?
The immune system is a complex system of cells, organs and tissues that work together to protect the body from potential harm by recognizing and responding to foreign substances, such as viruses, bacteria, fungi and parasites. Humans have two types of immunity, innate and acquired.
Innate immunity refers to the protective mechanisms that you are born with, including skin, tears, stomach acid and mucous membranes, all of which are ready to protect the body on short notice (Figure 1). All inner and outer surfaces of the human body are key components of the innate immune system that prevents germs from entering the body and prevents viruses and bacteria from multiplying.
Acquired immunity, on the other hand, requires exposure to a disease, which causes the immune system to produce antibodies that are specific to the invader. This can come from natural immunity through infection with an actual disease, or via a vaccine-induced immunity, which introduces a weakened or killed form of a disease into the body.
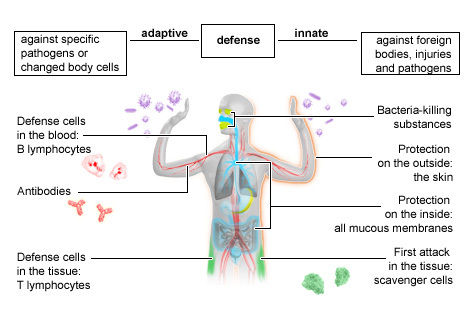
Reprinted from National Library of Medicine (2023). In Brief: The Innate and Adaptive Immune Systems. https://www.ncbi.nlm.nih.gov/books/NBK279396/
Nutrition
Nutrition can significantly impact immune function. The foods that we eat and drink contain numerous energy-giving nutrients, as well as non-nutrients, which are substances that do not provide vitamins or minerals and contain little to no calories but still support good health. Both nutrients and non-nutrients have specific roles in regulating metabolism and other critical processes, including immune signaling (the process by which immune cells communicate with other cells) to shield the body. Consuming a dietary pattern that is high in nutrients with immunomodulatory properties (i.e., substances that interact with the immune system and alter the body’s immune response) can serve to strengthen the immune system and keep it in good working order. Unfortunately, the opposite is also true: Inadequate nutrition can impair immune system development, leaving the body less protected against chronic inflammation, allergies and infections. This is known as immune incompetence.
Protein-rich foods, for example, assist in the synthesis of antibodies and contain antiviral properties, while tomatoes, green vegetables and mushrooms can help build disease resistance when consumed regularly. Water intake is also crucial for reducing illness risk, as it facilitates the movement of nutrients to all regions of the body (including elimination), aids in the oxygenation of cells and keeps the mucous membranes moist, thereby reducing the risk of cold and flu. Below is a list of common foods and nutrients and the roles they may play in supporting optimal immune system function.
It’s important to note that consuming a single food or food group is not as important as eating a variety of foods that contribute overall to a healthy immune system, as is evident when considering the various mechanisms of the sample foods described below.
| Common Foods and Nutrients | Mechanism of Action |
| Vitamin C | Helps the epithelial barrier function against infections Aids in the development of white blood cells |
| Citrus fruit (flavonoids) | Reduces inflammation |
| Almonds | Contain antioxidants Supports the production of T-cells (a type of white blood cell) |
| Tea | Supports the synthesis of immunoregulatory cytokines |
| Broccoli | Has anticancer and anti-inflammatory properties |
| Garlic | Activates natural killer cells (cells that directly destroy infected cells) |
| Eggs | Contain antioxidants that neutralize harmful free radicals to prevent damage to cells and tissues |
Exercise
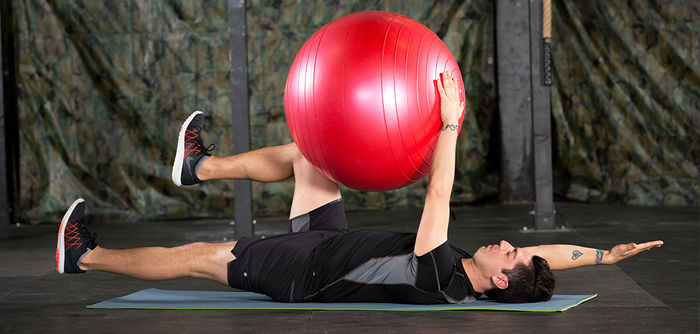
The mental and physical health benefits of exercise are often discussed, but have you ever considered how moving more affects your immune system? Interestingly, the immune system responds well to exercise in many ways. According to a recent literature review, moderate-to-vigorous intensity exercise bouts of less than 60 minutes enhance the immune system’s ability to recognize foreign invaders, including viruses, bacteria and cancerous cells. In addition, habitual exercise improves immune system regulation and delays immune dysregulation that occurs with age. Over time, exercise also has a cumulative effect in helping prevent atherosclerosis and the onset of cancer. In contrast, physical inactivity has a negative impact on the immune system such that consequences of inactivity, including muscle dysfunction and the accumulation of fat cells, can adversely affect both innate and adaptive immunity.
Stress
Stress can be defined as the body’s response to an event that exceeds the perceived ability to cope, resulting in overload. But, have you considered how the effects of everyday stressors might be impacting your immune system? Negative emotions and stress can dysregulate the immune response by interfering with the sensitive interplay taking place among the immune, endocrine and central nervous systems. Chronic stress can dysregulate or suppress immune responses by causing low-grade inflammation and suppressing the function of immunoprotective cells. In healthy individuals, the pro-inflammatory effects of stress are countered by hormones that help regulate inflammation and the immune system, which are also activated by stress. In people experiencing chronic stress, however, the effects of these hormones are diminished, and the pro-inflammatory mechanisms go unchecked. This is called glucocorticoid resistance.
Smoking
Another key lifestyle factor that can impact the functionality of your immune system is smoking. Smoking affects both innate and adaptive immune responses. However, while innate responses return to normal after smoking cessation, the changes to adaptive immunity are longer lasting. Smoking compromises immunity to bacterial infections and causes inflammation, with current smokers having an increased inflammatory response to bacterial infections, and has long-lasting effects on T cell responses. (T cells are white blood cells found in bone marrow.)
In other words, smoking not only causes various diseases, but it also disrupts immunological homeostasis and interferes with the normal defense functions of the immune system. In addition, the immunosuppressive effects of smoking enable tumor growth by weakening tumor-fighting cells (natural killer cells, T cells, B-lymphocytes and macrophages), rendering them ineffective.
Sleep
According for the Centers for Disease Control and Prevention, most adults need at least seven hours of sleep per night. However, one in three Americans reports not meeting this recommendation. While not getting enough sleep occasionally may not have dire consequences, when a lack of sleep occurs consistently over time it may lead to a variety of health problems and worsen others. For example, sleep profoundly impacts inflammatory and immune responses that protect against age-associated immune disorders such as neurodegenerative diseases, cancer and cardiovascular disease. You may have firsthand experience of the connection between sleep and the immune system, as you may have felt more tired or an increased desire to sleep when your body is fighting an infection. In addition, a good night’s sleep is often recommended as the best medicine for infectious disease.
Chronically deficient sleep can increase the risk for developing disease. On the other hand, achieving adequate sleep can improve disease risk. In addition, research shows that adequate sleep supports the bodily systems that produce blood and the development of new cells that can identify and fight harmful pathogens.
Loneliness
Loneliness can be described as the feeling when the need for human connection is not adequately met, or when a person’s social network does not align with their preferences. At the individual level, loneliness is associated with greater risk of stroke, dementia, anxiety, depression, cardiovascular disease and premature death. In fact, the mortality impact of being socially disconnected is greater than that associated with physical inactivity and obesity. The Surgeon General of the United States has even stated that the mortality impact is similar to that of smoking 15 cigarettes per day.
Loneliness does so much harm because it is associated with a heightened stress response, poor health behaviors and inadequate physiological repairing activity, all of which can impact both metabolic and immune regulation. Immune response dysregulation is caused by altered levels of inflammatory cytokines (proteins that promote inflammation), chemokines (signaling proteins that tell cells in which direction to move) and immunoglobulins (proteins that help the body fight infection). Altered antibody responses against vaccines and viruses and immune system cell activity may also contribute to dysregulation. These altered interactions, along with altered glycemic control, lipid metabolism, metabolic syndrome and body composition, have led researchers to describe loneliness as an immunometabolic syndrome. Loneliness not only impacts your psychological state, but it can also affect systemic regulatory pathways within your body and your mental and physical well-being.
Conclusion
The immune system is the body’s defense structure against foreign invaders. The first line of defense for supporting a healthy immune system is leading a healthy lifestyle, which includes a healthy diet, physical activity, stress management, avoiding smoking and the use of other risky substances, restorative sleep and positive social connections. The relationship between lifestyle factors and the immune system is evident, and your lifestyle can impact your immune system either positively or negatively. When you lead a healthy lifestyle, your immune system functions properly, but when your health is poor as related to the factors described above your immune system is not optimized. While our immune system may not be “boosted” beyond functioning properly—a term commonly used in marketing and social media posts—there are definite steps you can take to ensure your body is operating to its full capacity.
To learn more about innovative strategies for holistic well-being, check out Holistic Wellness: Transformative Strategies for Client Well-being (worth 0.1 ACE CECs). In this course, you’ll delve into the concept of wellness as a multidimensional construct and discover strategies to enhance your clients’ physical fitness while simultaneously promoting mental, emotional and social well-being.




 by
by 









 by
by