How Much Protein Does Grandpa Really Need?

Large public health organizations like the World Health Organization (WHO) and the Food and Agriculture Organization of the United Nations (FAO) make recommendations for protein intake as part of their efforts to improve global health. Two numbers are often used in this context: Estimated Average Requirement (EAR) and Recommended Daily Allowance (RDA). The EAR refers to an intake value that is estimated to meet the requirement of half the healthy individuals in a group, and by definition implies a high risk of inadequacy (i.e., only 50 percent of a healthy population will have a higher intake). The RDA is set at an intake level that should meet the needs of about 97 percent of healthy individuals. The current EAR for protein intake in healthy adults according to the WHO and Institute of Medicine is 0.66 grams per kilogram of bodyweight per day, and the RDA is 0.8 grams per kilogram of bodyweight per day.
Recommendations for healthy adults are generally derived from studies conducted mainly in younger adults. This is potentially problematic for a number of reasons. For example, compared with younger adults, the muscles of older adults are less sensitive to smaller doses of protein and appear to require a greater amount of protein to fully stimulate muscle protein synthesis.
Inadequate protein intake results in loss of lean body mass, decreased muscle function, and even an impaired immune response to stress and infection. Previous research has shown protein intakes at the current RDA can lead to negative nitrogen balance and loss of muscle mass in elderly individuals. Due to this, some recommendations now suggest an intake of 1.2 to 1.5 grams of protein per kilogram of bodyweight per day for certain older populations. Observational research has found associations in elderly people between a greater dietary protein intake and improved health.
Current recommendations are based on data from nitrogen balance studies, which are a type of study that attempts to determine protein requirements by measuring the amount of nitrogen (a key component of amino acids, the building blocks of protein) that is ingested and the amount that is excreted (via sweat, urine, feces, hair and skin).
Unlike carbon, oxygen and hydrogen (other building blocks of amino acids), nitrogen doesn't turn into gases and water during metabolism, so it can be measured as a specific marker of protein balance. Being in negative nitrogen balance means that the amount of nitrogen excreted from the body is greater than the amount of nitrogen ingested, and is associated with wasting diseases and muscle catabolism, while positive nitrogen balance means that the amount of nitrogen excreted from the body is less than the amount of nitrogen ingested, and is associated with growth and muscle buildup. The use of nitrogen balance to determine optimal protein intake dates back over 100 years.
However, the nitrogen balance method has several limitations. For instance, variations in overall body nitrogen and amino acid metabolism can lead to a change in nitrogen balance, with or without a change in intake. If excretion is changing without a change in intake, it becomes difficult to determine whether or not the effect is due to the dietary protein intake, because this method is basing conclusions on specific dietary protein intakes. Also, testing requires five to 10 days of adaptation to each level of amino acid by a participant, and complete collection and quantification of all sources of nitrogen excretion (mostly in urine and feces, but also sweat) is difficult.
Which Amino Acids are Essential, Nonessential and Conditionally Essential?
Essential amino acids are those that cannot be made by the body. These are histidine, isoleucine, leucine, lysine, methionine, phenylalanine, threonine, tryptophan, and valine. In contrast, non-essential amino acids can be made by the body, even if we do not consume them. These are alanine, asparagine, aspartic acid and glutamic acid. Finally, conditionally essential amino acids are only essential during times of increased stress or illness, or in people that do not synthesize them in adequate amounts. These include arginine, cysteine, glycine, glutamine, proline, serine and tyrosine.
Recent studies using the IAAO method in older women (older than 65 years and older than 80 years) and young men have found the protein requirement to be higher than the current RDA. The primary goal of the current study was to use the IAAO method to determine protein requirements for healthy men older than 65, and to compare that with the needs of older women and younger men, as previously determined by the same method.
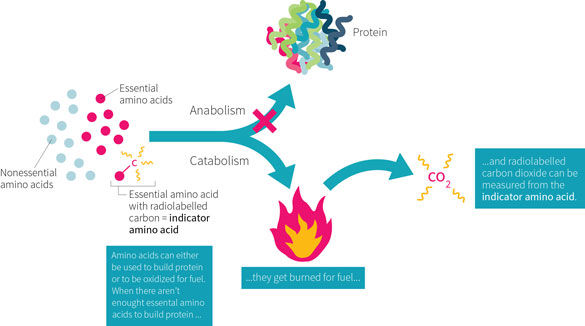
An alternative method for studying protein needs is the indicator amino acid oxidation (IAAO) method, which is shown in Figure 1, above. This method is based on the concept that when one essential amino acid (EAA) is deficient for protein synthesis, then all other EAAs, including the “indicator” amino acid, will be oxidized. This is because the deficient amino acid becomes the limiting step in protein synthesis. The indicator amino acid (often phenylalanine, though lysine or leucine can also be used) is “labeled” with a stable isotope (like a tracking device). The appearance of the label in exhaled carbon dioxide is used as an indicator of a protein or amino acid requirement. This method was originally developed to determine requirements for individual amino acids. Researchers would vary the levels of one EAA and measure oxidation of the tracer. However, in the current study, the researchers varied the levels of all EAAs (except phenylalanine and tyrosine) in parallel, then observed how much of the other EAAs it takes for phenylalanine oxidation to drop, as measured by the tracer. Since there is no storage of amino acids, the indicator is either incorporated into protein or oxidized. This method is non-invasive, doesn’t require a week of adaptation at a set protein level, and can be measured through breath and urine samples.
Current recommendations for protein intake may be underestimated, particularly for older adults. This study used newer and potentially more accurate testing methodology to determine protein requirements for men over the age of 65.
Who and What was Studied?
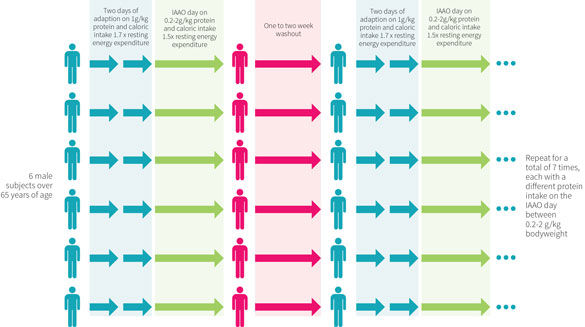
The study design is depicted in Figure 2, above. Participants were randomly assigned to receive test protein intakes ranging from 0.2 to 2.0 grams per kilogram of bodyweight per day. Each participant was included in seven studies, with each three-day study period separated by one to two weeks. During each three-day study, two adaptation days were followed by the IAAO study on the third day.
On the two adaptation days, participants received a lactose-free milkshake maintenance diet that supplied 1.0 gram of protein per kilogram of bodyweight per day and total calorie intake of 1.7 times each participant’s measure resting energy expenditure (REE; this is standard for weight maintenance, with the activity factor of 1.7 calculated to consider general daily activity). The daily diet was consumed as four equal meals. The set protein intake of one gram per kilogram was chosen because previous research showed that varying the protein intake had a significant effect on amino acid kinetics on the study day. This implies that the body can adapt over time. Using a high-protein run-in with a one-day test period could artificially inflate protein requirements because there is no time for adaptation to lower protein levels. Lactose-free milkshakes were chosen because five of the six participants reported being lactose intolerant.
On the third study day, the IAAO testing was performed. Participants were provided protein intakes ranging from 0.2 to 2.0 grams per kilogram of bodyweight, after a 12-hour fast. The food was consumed as eight separate meals given hourly, and was not exactly appetizing. The experimental diet consisted of Tang and Kool-Aid, grape seed oil, an amino acid mixture similar to egg protein, and protein-free cookies. Caloric intake was provided at 1.5x REE, with the carbohydrate content of the diets being adjusted according to the protein intake in order to keep the calorie intake the same. The study diet consisted of 40 percent fat, 37 to 57 percent carbohydrate, and 3 to 37 percent protein. Phenylalanine was used as the “indicator” amino acid, and thus intake was kept constant at 30 milligrams per kilogram of bodyweight per day across all studies. Additionally, tyrosine was also kept constant at 40 milligrams per kilogram of bodyweight per day to ensure adequate tyrosine intake, which can be formed from phenylalanine. If there was inadequate tyrosine intake, some of the phenylalanine would go to making tyrosine and change the results of a given test intake.
Six men aged 65 years or older were tested seven times with protein intakes ranging from 0.2 to 2.0 grams per kilogram per day. The non-invasive indicator amino acid oxidation (IAAO) method was used to determine protein balance.
What Were the Findings?
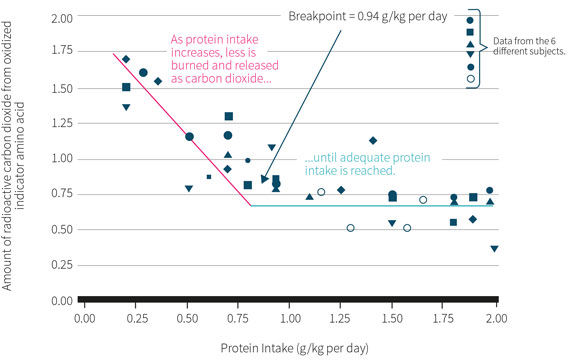
Figure 3, above, summarizes the study findings. The rate of the labeled CO2 released from the oxidation of phenylalanine (the indicator amino acid) declined with increasing protein intakes up to 0.94 grams per kilogram of bodyweight per day. Additional increases in protein intakes did not result in changes in the labeled CO2 values, meaning there were no additional increases in the incorporation of phenylalanine for protein synthesis. This would imply an estimated average requirement (EAR) of 0.94 grams per kilogram of bodyweight, with an RDA of 1.24 grams of protein per kilogram per day required to ensure the needs of 97 percent of the population.
The researchers also compared data from this study to previous studies they had conducted in older women (older than 65 years) and young men using the same IAAO method. When expressed in grams per kilogram of body weight, there were no differences in protein requirements between the three groups (0.94 grams per kilogram). However, when comparing per kilogram of fat-free mass (FFM) the protein needs were higher in older men and women (1.6 g/kg FFM) compared with young men (1.14 g/kg FFM).
Using the indicator amino acid oxidation method, the estimated average protein requirement and RDA for older men were 0.94 and 1.24 grams per kilogram per day, respectively.
What Does the Study Really Tell Us?
This study suggests that current recommendations for dietary protein intakes (0.66 g/kg/d for the EAR and 0.8 g/kg/d for the RDA) may be an underestimation for older adults.
The IAAO method, which has been compared to the nitrogen balance method, suggests that an intake between 0.94 g/kg/d and 1.24 g/kg/d may be more suitable for a general recommendation. Limitations of the the study include the small sample size of six men. But these results concord with previous studies by the same group, where similar results were observed, implying that protein requirements are not affected by age or sex when compared on a bodyweight basis.
However, there do appear to be increases in protein requirements on the basis of FFM in older, compared with younger, adults. This could be due to muscle protein synthesis being impaired in older adults compared with younger adults, with greater protein intakes being required to lead to comparable protein synthesis rates. Additionally, the study design, and more specifically this method, does not allow time for the body to adapt to lower protein intakes, which can occur in response to consistently low protein intakes.
The Big Picture
This paper is the third in a series of studies looking at the protein needs of older adults. Previous data in older women (older than 65 years) showed similar protein requirements compared to this study (an EAR of 0.96 g/kg compared to 0.94 g/kg found in this study). On the basis of fat-free mass, however, the estimated protein needs are higher in older adults (about 1.6 g/kg FFM) compared with younger adults (1.14 g/kg FFM). This would be expected, because FFM is typically a smaller percentage of total bodyweight on older adults.
There are a few potential reasons for the increased dietary protein requirements in older people on the basis of FFM. Compared with younger adults, the muscles of older adults are less sensitive to protein and require a greater amount of protein to fully stimulate muscle protein synthesis. Also, daily protein turnover is lower in older adults than it is in younger adults. This is due to a decreased contribution of skeletal muscle to whole-body protein breakdown. Skeletal muscle supplies a significant percentage of the amino acids required to promote whole-body protein synthesis, and this decreased contribution could be what’s causing an increase in required dietary protein intake.
Another study by the same group of researchers in octogenarian women also found the current EAR and RDA to be underestimated, with the average protein requirement (EAR) being 0.85 grams per kilogram and an adequate allowance (RDA) value to be 1.15 grams per kilogram. Beyond the IAAO studies, a number of observational studies provide support for optimal protein intakes being greater than current recommendations. For further reading, two recent reviews on the subject are suggested.
Much of the existing body of research on protein requirements has used nitrogen balance studies. However, the IAAO method has become widely accepted as a valid model and allows for a less invasive experimental design for protein requirement studies. When an essential amino acid is missing or limited in the diet, protein synthesis is then limited by that particular amino acid. IAAO uses the oxidation of carbon as an endpoint, in contrast to nitrogen balance studies that measure nitrogen intake and excretion. This method also allows research in populations less commonly studied, such as pregnant women and children, for whom exposure to dietary protein deficiency for up to 10 days in a row during testing would be clearly unethical. An important limitation to this study design is that it does not allow for a period of adaptation to a low-protein diet. Evidence from both humans and animals suggests the body can adjust metabolic processes in order to maintain nitrogen balance.
Frequently Asked Questions
Does it matter what type of protein I consume when trying to meet the RDA?
Yes. Dietary protein recommendations are made with the assumption that it consists of “high quality” protein. Protein quality refers to the balance of amino acids, digestibility of the protein, and the availability of the absorbed amino acids for protein synthesis. Lower quality proteins will require a greater dietary intake in order to meet the body’s needs for essential amino acids. People may be familiar with the Protein Digestibility Corrected Amino Acid Score (PDCAAS), but a newer and more accurate estimation of protein quality is the Digestible Indispensable Amino Acid Score (DIAAS), recently proposed by the Food and Agriculture Organization. DIAAS scores for animal proteins (e.g., milk, eggs, and beef) are well above 100 percent, while vegetable proteins are usually less than 80 percent, with the exception of soy. Combining incomplete vegetable proteins such as rice and beans can be used effectively to provide the body with its complete needs.
How does recommended protein intake compare with actual protein intake?
This is difficult to answer because large-scale observational studies are notoriously inaccurate, but there is likely a fairly large variation of intake. One study in older women (aged 60 to 90 years) found the average protein intake to be 1.1 grams per kilogram of bodyweight per day, though 25 percent of the cohort consumed less than the RDA of 0.8 grams per kilogram of bodyweight. Another study in older men and women reported an average intake of around 70 grams per day, with a standard deviation of nearly 25 grams, indicating a very wide range of individual intakes.
What Should I Know?
Use of a newer (and possibly, but not definitely, better) method for determining dietary protein requirements suggests that the current intake recommendations for older adults of 0.66 grams per kilogram of bodyweight per day for the estimated average requirement (EAR) and 0.8 grams per kilogram of bodyweight per day for the recommended daily allowance (RDA) may be too low. Although this study used a very small sample size, when combined with previous research by the same group, a more accurate recommendation for this population would be 0.94 g/kg as an EAR and 1.24 g/kg as an RDA. More research is needed, however, before it would be prudent to increase the EAR and RDA.
Reproduced with permission from Examine.com. All rights reserved.
More Articles
- ProSource™: July 2016
ACE-SPONSORED RESEARCH: Can Elevation Training Masks Improve Performance?
- ProSource™: July 2016
Functional Anatomy Series: The Shoulders
Health and Fitness Expert
- ProSource™: July 2016
Coaching Behavior Change: Dealing With Discord
Health and Fitness Expert
- ProSource™: July 2016
How to Write a Fitness Blog Post Worth Reading
Health and Fitness Expert